What To Know About Crohn’s Disease And Cramps
Here are nine things you should know about Crohns disease and cramps:
1. Abdominal cramps can occur anytime. Cramping can start during a flare or when youre in remission, says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio. When Crohn’s disease is active, inflammation can change nerve and muscle function in the intestines, Dr. Philpott says. Even after inflammation is reduced, the functioning of the gastrointestinal tract remains altered.
2. Cramps can be caused by a variety of sources. Pinpointing the origin of cramps can help you treat the source, says Susan Coe, MD, a gastroenterologist with the Gwinnett Medical Center in Lawrenceville, Georgia. For example, if active Crohns disease is causing your cramps, treatment should be geared to reducing inflammation and treating any Crohns disease-related complications, such as a bowel blockage or fistulas, Dr. Coe says. Your doctor may recommend medications to help ease your symptoms during a flare and put the disease into remission afterward. If your cramping is from a stricture, which is the narrowing in a section of the colon, a low-residue, low-fiber diet can help, says Sandra M. Quezada, MD, an assistant professor of medicine in the division of gastroenterology and hepatology at the University of Maryland Medical Center in Baltimore. Foods low in fiber dissolve and pass through narrowed areas of the colon more easily, she says.
Diagnosing Back Pain In Ulcerative Colitis
Diagnosing back pain as a symptom of ulcerative colitis can be tricky. Back pain can be attributed to a number of causes, including injury and strain. Because of the other potential causes, some people may not think to mention their backaches when seeking care for their UC. Whats more, back pain may develop years before UC does, making it more challenging to note the connection between the two.
If your doctor suspects that your UC has led to axial arthritis or ankylosing spondylitis, they will likely ask you to come in for a physical exam and tests. During this exam, they may test the range of motion in your spine and gauge your ability to take a deep breath. The doctor may also try to pinpoint the location of your pain by moving your legs or pressing on certain areas of your pelvis.
Radiographic tests are also commonly used to diagnose axial spondyloarthritis. Your doctor may use an X-ray to check for damage to your bones or joints. If no inflammatory damage is visible on the X-ray, your doctor may also order an MRI scan to get a more detailed view of your soft tissue and bones. An MRI scan can be particularly helpful, as it can allow doctors to catch and start treating your axial arthritis or AS before damage becomes extensive.
Axial Arthritis And Crohns Disease
Axial arthritis affects roughly 19 percent of people with Crohns disease. It tends to appear in certain people more often than others. Males, people in their teens and 20s, and those who have family members with spondyloarthritis are at an increased risk of developing the condition themselves.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.
These symptoms appear as the result of enthesitis inflammation of the entheses, or areas where ligaments and tendons enter the bone. This can cause enthesopathy, or the erosion of the bone where it attaches to soft tissue.
Also Check: How To Stop My Lower Back From Hurting
He Had Recurring Pain For Nearly A Decade
-
Send any friend a story
As a subscriber, you have 10 gift articles to give each month. Anyone can read what you share.
Give this article
The pain woke the 52-year-old physician from a dead sleep. It was as if all the muscles in his right leg, from those in the buttock down his thigh to the very bottom of his calf, were on fire. He shifted slightly to see if he could find a more comfortable position. There was a jag of pain, and he almost cried out. He glanced at the clock: 4 a.m. In just three hours he would have to get up. He had a full day of patients to see. Massage didnt help. He couldnt get comfortable lying flat, so finally he moved to the living room, to a recliner. Only then, and only by lying completely still, did he manage to get the pain to abate. He drifted off, but never for long. The searing pain in his leg and buttock slowly eased, and by the time his alarm went off, he could stand and walk though his muscles still ached and he had to baby his right leg, causing a limp.
Between patients, he arranged to see his own doctor. Hed had pain off and on in his buttocks, one side or the other, for more than a year. The pain was in the middle of each cheek and was worse when he was sitting and at the end of the day. Walking to and from his car on the way home was brutal. And then, as mysteriously as it came, it would disappear only to come back a week or two later.
Joints In Your Arms Or Legs
Diagnosis of joint problems in wrists, knees, elbows or hands and enthesitis is based on signs of inflammation and ruling out other forms of arthritis. Your doctor may ask you these questions to understand your symptoms: Do you have joint pain? When you wake up in the morning do you notice stiffness in your joints for morethan 30 minutes?
Studies have shown that a large proportion of people with Crohns and Colitis experience back pain and joint pains without inflammation . Back pain has been reported by 4 in 10 people and almost a third of people report knee pain. Almost a quarter of people have reported pain in the hand and finger joints and 2 in 10 shoulder pain.
I found a course in pain management really effective in helping me to be kinder to myself and understand what I need to do to minimise my joint pains.
Alison
Because of the different patterns of activity there are different treatment approaches depending on the type of arthritis you have and if you are having a flare-up of your gut problems.
Read Also: How To Heal Strained Lower Back
Routine Screening To The Rescue
When the physician turned 60, he scheduled a colonoscopy, a recommended test to screen asymptomatic individuals over 50 for colon cancer. He had one at 50 it was completely normal. When it was time for his next exam, the doctor who did it the first time had retired, so he asked a friend, Dr. Erick Chan, a gastroenterologist, to perform the test.
He was still a little foggy from the anesthesia when Chan came by with what the physician assumed would be the usual report of normal results. He was wrong. I took some biopsies, and well wait to see what they show, Chan said. But I have to tell you, it didnt look normal. The test had been routine until Chan got close to the spot where the colon and the small intestine connect, a structure known as the ileocecal valve. Chan noticed that the valve looked a little asymmetric.
As Chan advanced his scope, he could see that the valve was distorted by scar tissue so much so that the connection was too narrow for his instrument to enter. Bringing his scope as close to the opening as he could, he saw that the tissue on the other side was an angry red and dotted with ulcers. They would have to wait for the biopsies to come back, but Chan suspected Crohns disease. Thats impossible, the man responded. He had no G.I. symptoms at all. No pain, no diarrhea, no blood in his stools. How could he possibly have Crohns?
What Is Crohns Disease Exactly
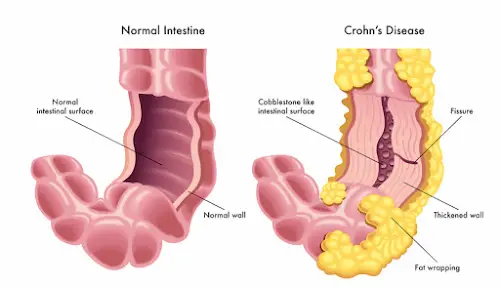
Crohns disease is one form of inflammatory bowel disease , which includes other conditions such as ulcerative colitis, according to the U.S. National Library of Medicine . IBD happens when your immune system mistakenly attacks healthy cells in your digestive tract and causes chronic inflammation, setting off a slew of symptoms, as well as possible complications if the disease isnt treated.
Researchers believe this autoimmune reaction occurs when your immune system has an abnormal response to bacteria in your digestive tract, but why this happens isnt entirely understood. Over time, chronic inflammation can cause visible damage to the digestive tract, which can be seen on scans, Benjamin Lebwohl, M.D., gastroenterologist and associate professor of medicine at Columbia University Vagelos College of Physicians and Surgeons, tells SELF.
Crohns in particular causes inflammation anywhere in your digestive tract . However, it most commonly affects the small intestine and the large intestine .
Its not clear why some people get Crohns disease and others dont, but experts suspect genetics might be involved since the condition can run in families, according to the NLM. In fact, scientists have found more than 100 genes that are associated with having IBD, but more research is needed to understand the link1.
Recommended Reading: Which Mattress Is Good For Lower Back Pain
Back Pain As A Symptom Of Crohns Disease
Back pain is a relatively common symptom among people with Crohn’s disease. In one study, over half of people with Crohns disease reported having low back pain, and 45 percent showed signs of sacroiliitis . Similarly, a 2008 study found that in the majority of cases, people with Crohns will report having inflammatory low back pain if their provider takes a detailed history with the right questions.
That said, a doctor may not even suspect that a person with back pain has Crohns unless they also experience GI problems. These characteristic symptoms of Crohn’sinclude:
- Abdominal pain
- Malnutrition
- Weight loss
When a person with Crohns experiences backaches, they may not associate the pain with their digestive problems nor think to mention it to their doctor. If you do have back pain, its important that you share it with your doctor even if you dont suspect that its related to Crohns.
What Is Crohns Disease
Crohns disease, also called regional enteritis or ileitis, is a lifelong form of inflammatory bowel disease . The condition inflames and irritates the digestive tract specifically the small and large intestines. Crohns disease can cause diarrhea and stomach cramps. Its common to experience periodic disease flare-ups.
Crohns disease gets its name from American gastroenterologist Dr. Burrill Crohn . He was one of the first physicians to describe the illness in 1932. Ulcerative colitis is another commonly diagnosed IBD.
You May Like: What Is Good For Arthritis Back Pain
Diagnosing Back Pain In Crohns Disease
Diagnosing back pain as a symptom of Crohns disease can be tricky. Back pain can be attributed to a number of causes, including injury and strain. Because of the other potential causes, some people may not think to mention their backaches when seeking care for their Crohns. Whats more, back pain may develop years before Crohns does, making it more challenging to note the connection between the two.
If your doctor suspects that your Crohns has led to axial arthritis or AS, they will likely ask you to come in for a physical exam and tests. During this exam, they may test the range of motion in your spine and gauge your ability to take a deep breath. The doctor may also try to pinpoint the location of your pain by moving your legs or pressing on certain areas of your pelvis.
Radiographic tests are also common when it comes to diagnosing axial spondyloarthritis. Your doctor may use an X-ray to check for damage to your bones or joints. If no inflammatory damage is visible on the X-ray, your doctor may also order an MRI scan to get a more detailed view of your soft tissue and bones. MRI can be particularly helpful, as it can allow doctors to catch and start treating your axial arthritis or AS before damage becomes extensive.
Back Pain And Ulcerative Colitis
| | |
Research indicates that nearly 25 percent of people with inflammatory bowel disease including ulcerative colitis and Crohns disease experience chronic lower back pain. Ankylosing spondylitis and axial arthritis both of which can cause back pain are two common causes of back pain for people with UC.
That said, a doctor may not suspect that a person with back pain has UC unless they also experience gastrointestinal symptoms. If you do experience back pain, its important to let your doctor know even if you dont suspect its related to UC. They will be able to determine the cause of your pain and work with you to find the best way of managing it.
- Weight loss
A person having backaches may not realize theyre related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
Don’t Miss: How To Get Rid Of Lower Back Hair
The Link Between Crohns And Arthritis
Some research suggests an overlap between Crohn’s disease and other immune-mediated inflammatory diseases, such as psoriatic and rheumatoid arthritis. An analysis published in September 2020 in Wiener Klinische Wochenschrift found that people with psoriatic arthritis tended to also have Crohns disease or ulcerative colitis. A research review published in June 2020 in BMC Gastroenterology found that people with inflammatory bowel disease , including Crohns disease and ulcerative colitis, have a significantly increased risk of rheumatoid arthritis.
“It is believed that the chronic inflammation in the intestines or colon can trigger the immune system to start an inflammatory process in the joints or tendons,” says Michael R. Cannon, MD, a rheumatologist with Arthritis Consultants of Tidewater in Virginia Beach, Virginia.
High inflammation manifests in both diseases, and one theory is that bacteria may be behind it. Research published in February 2017 in Science Translational Medicine found large amounts of a specific type of E. coli in the feces of people with Crohns disease and spondyloarthritis . In the same study, researchers found that the bacteria affected Th17 cells, which mediate inflammatory responses.
RELATED: Could a New Diet Focused on Restoring the Gut Microbiome Reduce IBD Symptoms?
Apakah Benar Russia Ban Crypto
Russia merupakan negara dengan aktivitas penambangan Bitcoin terbesar ketiga di dunia setelah Amerika Serikat dan Kazakhstan.
Meski begitu, nama Russia kini tengah ramai diperbincangkan karena dibannednya aktivitas cryptocurrency di negara tersebut.
Namun sebenarnya hal itu belum benar-benar terjadi di Russia. Melainkan hanya usulan yang diberikan oleh pihak Bank sentral Rusia pada Kamis 20 Januari 2022.
Mereka mengusulkan pelarangan terhadap penggunaan dan penambangan mata uang kripto di wilayah Rusia.
Alasannya adalah karena penggunaan mata uang Crypto bisa menjadi ancaman terhadap stabilitas keuangan, kesejahteraan warga, dan kedaulatan kebijakan moneternya.
Also Check: Can A Pinched Nerve In Your Back Cause Leg Pain
Diagnostic Tests/lab Tests/lab Values
The diagnosis of Crohns disease is made by ruling out other potential causes to explain the patients signs and symptoms. Some of the tests include blood tests, fecal occult blood test , colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.
The blood tests are used to check for anemia which would indicate inflammation within the body, infection, and antibodies that might be present with individuals with inflammatory bowel disease.
The FOBT assesses an individuals stool sample for the presence of blood.
A colonoscopy allows the doctor to take a biopsy or tissue sample to determine if there is a presence of any granulomas which are common with Crohns disease and not ulcerative colitis.
The flexible sigmoidoscopy allows the doctor to assess the last portion of the colon for any biopsy samples. This allows the doctor to determine if there is any inflammation or bleeding amongst the intestines.
Barium enemas allow the doctors to assess the intestines via x-ray. The barium coats the inner lining of the GI tract to allow the lining to be visible on the x-ray.
A CT of the GI tract allows a quick look at the entire bowel in a way that cannot be seen in other diagnostic tests. This helps to assess for blockages, abscesses or fistulas.