Ibp Versus Mbp Key Features
It is important to distinguish between IBP and MBP as early as possible in the disease course because management and treatment of the two types of back pain are very different. IBP is differentiated from MBP by key characteristic features identified by experts from the Assessment of SpondyloArthritis international Society 1) , including chronic back pain of3 months in duration , insidious onset at age< 40 years, improvement with exercise, no improvement with rest, pain at night , and elevated acute phase reactants . IBP is present in axSpA and the axial form of PsA, and is typically associated with early pain onset localized to the axial spine, sacroiliac joints, and buttocks . MBP is identified by first ruling out red flags and symptoms, including trauma, unexplained weight loss, neurological signs, age> 50 years, fever, intravenous drug use, long-term steroid use, and history of cancer however, there is no clear evidence about which are clinically relevant . Onset of MBP can occur at any age and can be acute pain may worsen with movement and improve with rest .
Alternate Heat And Cold
When your muscles are sore, try alternating hot and cold compresses on the sore areas. Heat helps alleviate pain and tension by loosening the muscles around the joints and increasing flexibility and circulation. Cold, on the other hand, helps reduce inflammation and dull pain.
Note that because heat and cold are psoriasis triggers for many people who also have psoriasis, you may need to avoid one or the other of these treatments. You know your body best, so choose based on that knowledge.
Psoriatic Arthritis And Back Pain
Learn more about axial arthritis or spondylitis, which causes back pain and may affect your treatment for PsA.
When you think of psoriatic arthritis , you may imagine skin symptoms or the commonly affected joints, like the fingers, knees, ankles or elbows . However, for many people with the disease, back pain can become a symptom as well. When the spine is affected, its known as axial arthritis or spondylitis. Spondylitis affects the spine and sacroiliac joints, which are located at the bottom of the back.
Who Does Spondylitis Affect?
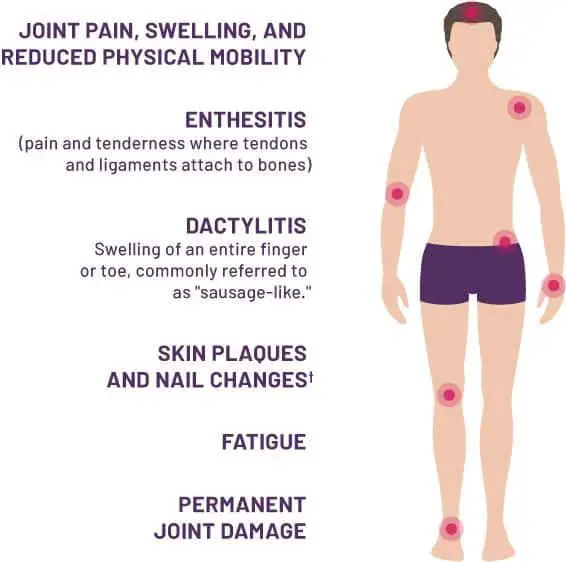
Many people with PsA have axial arthritis and most of them will have a mix of peripheral and axial arthritis. A much smaller number of people with PsA can have inflammation primarily in the axial area without peripheral symptoms.Axial involvement is usually a late-onset feature of PsA, but not always. Studies show that most PsA patients with spondylitis can have back symptoms for up to 10 years before diagnosis is made.Other symptoms of PsA that people with axial disease may have include inflammation where ligaments and tendons insert into bones inflammation of an entire finger or toe skin disease pitting and lifting of nails from the nailbed eye inflammation and inflammatory bowel disease .Since the treatment for PsA with axial involvement may be different than for PsA with only peripheral symptoms, it is important to know the signs and talk to your doctor about your back pain.
Mechanical Pain vs. Inflammatory Back Pain in PsA
Also Check: What Can I Do To Relieve Upper Back Pain
Who Will Be Responsible For My Healthcare
Youre likely to see a team of healthcare professionals.
Your doctor, usually a rheumatologist, will be responsible for your overall care. And a specialist nurse may help monitor your condition and treatments. A skin specialist called a dermatologist may be responsible for the treatment of your psoriasis.
You may also see:
- a physiotherapist, who can advise on exercises to help maintain your mobility
- an occupational therapist, who can help you protect your joints, for example, by using splints for the wrist or knee braces. You may be advised to change the way you do some tasks to reduce the strain on your joints.
- a podiatrist, who can assess your footcare needs and offer advice on special insoles and good supportive footwear.
What Treatment Is Right For Me
The type of treatment will depend on how severe your symptoms are at the time of diagnosis with the goal being to control the disease to the point of remission and avoid complications. Medications may need to be changed over time to continue to maintain control and avoid disease progression and systemic effects. Some early indicators of more severe disease include onset at a young age, multiple joint involvement, and spinal involvement. Good control of the skin is important in the management of psoriatic arthritis. In many cases, you may be seen by two different types of healthcare providers, one in rheumatology and one in dermatology.
Early diagnosis and treatment can relieve pain and inflammation and help prevent progressive joint involvement and damage. Without treatment psoriatic arthritis can potentially be disabling, cause chronic pain, affect quality of life, and increase risk of heart disease. It is important to update your healthcare provider when you have a change in symptoms or if your medication regimen is no longer effective.
Recommended Reading: How To Relieve Lower Back And Leg Pain
Swollen Joints Fingers And Toes
Often you’ll notice swelling in your knees, ankles, feet, and hands. Usually, a few joints are inflamed at a time. They get painful and puffy, and sometimes hot and red. When your fingers or toes are affected, they might take on a sausage shape. Psoriatic arthritis might affect pairs of joints on both sides of your body, like both of your knees, ankles, hips, and elbows.
Tips For Living With Plaque Psoriasis On The Lower Back
There are many strategies that people living with plaque psoriasis can use to help manage their symptoms and improve their quality of life. Many people find it helpful to take a lukewarm bath with oils, Epsom salts, or colloidal oatmeal2. Avoiding harsh soaps and hot water is important, however. Applying moisturizer or oils regularly to the skin throughout the day can be beneficial.
It is important for people living with psoriasis to try to figure out the triggers of their flare-ups, which are periods of time when symptoms get worse. Common triggers include sun exposure, stress, smoking, and skin injuries. Knowing what your personal triggers are will allow you to avoid them and help to prevent flare-ups.
Recommended Reading: Which Painkiller Is Best For Back Pain
Coping And Treating Skin Pain
Even when you cant avoid flares, you can find ways to cope and treat skin pain. Here are some self-care tips to help you manage pain.
Keep skin lubricated: Keeping your skin lubricated can prevent dry, itching painful skin. It can also reduce redness and heal skin. The National Psoriasis Foundation recommends heavy creams that lock in water. Make sure you are using moisturizers that are fragrance-and alcohol-free, as fragrances and alcohol may dry out skin.
Refrigerate creams: Keep creams and moisturizers in your refrigerator. This helps keep them cold so they can soothe burning and itching.
Soften scales: You can soften scales with lotions containing lactic, salicylic, or glycolic acids. These substances can break up dead skin cells that have built up on psoriasis plaques. Generously apply to skin at night and cover up with a plastic wrap overnight. This way the lotion stays and absorbs into skin better.
Try capsaicin: Check your drugstore for creams, lotions, and ointments containing capsaicin. Capsaicin is the ingredient in chili peppers that makes them hot. Products containing capsaicin block the nerve endings that cause pain. These products may also help reduce inflammation, redness, and scaling. However, there isnt enough research to confirm these benefits in the long-term or on the safety of capsaicin.
Cold therapy: Using cold packs confuses the brain. Your brain cannot feel the itch if you are feeling cold at the same time.
How Did I Get Toenail Psoriasis
It is not known exactly what causes psoriasis. The disease is known to have a strong genetic componenta third of all sufferers have a family history of psoriasis, and if an identical twin develops the disease it is 70% likely that the other twin will also develop itbut other factors also seem to have an effect.
Certain drugs and medications have been reported to cause psoriasis, and lifestyle factors such as drug and alcohol abuse, stress, smoking, and obesity are all known to exacerbate existing cases. Environmental factors such as excessive heat or dryness can also have this effect.
You May Like: Ibuprofen For Back Pain Dosage
Read Also: When Should I Go To The Hospital For Back Pain
What Complications Are Associated With Sacroiliitis
Left untreated, sacroiliitis causes a loss of mobility for some people. Untreated pain also can disrupt your sleep and lead to psychological conditions like depression.
Sacroiliitis associated with ankylosing spondylitis can progress over time. Over time, this type of arthritis causes the vertebrae in your spine to fuse together and stiffen.
An Overview Of This Condition
Psoriatic spondylitis is a type of psoriatic arthritis in which inflammation affects the spine and causes movement problems in the neck, low back, pelvis, and sacroiliac joints. Psoriatic spondylitis may also cause joint pain in the arms, legs, hands, and feet.
You May Like: Why Is My Lower Back In Severe Pain
What Is Psoriatic Arthritis
Psoriatic arthritis is a type of inflammatory arthritis that affects some patients who have the skin condition psoriasis, said Edwin Aquino, MD, a rheumatologist with Banner University Medical Center Tucson. Studies suggest that some people may be genetically predisposed to getting it as well.
While one-third of people who have psoriasis get psoriatic arthritis, many more develop it without having psoriasis. Psoriatic arthritis can start at any age, but it generally starts between the ages of 30 and 50. Theres no cure for psoriatic arthritis, thats why its important to discover it early on. Left untreated, it can permanently damage joints.
Three Signs Point To A Diagnosis Of Psoriatic Arthritis
Doug Brunk
LOS ANGELES, California If a patient with psoriasis presents with dactylitis, inflammatory back pain, and/or tendon inflammation, think psoriatic arthritis until proven otherwise.
Amanda Mixon speaks at the 19th Annual Fall Dermatology Conference of the Society of Dermatology Physician Assistants .
At the annual fall meeting of the Society of Dermatology Physician Assistants, Amanda Mixon, PA-C, said that psoriatic arthritis occurs in 20% to 30% of individuals with psoriasis, but my guess is that number is higher than that. Mixon practices at the Colorado Center for Arthritis and Osteoporosis, Longmont, Colorado. Psoriasis usually precedes PsA by 8 to 10 years, and PsA affects both genders equally, usually in the fourth decade of life. Genetic and environmental factors play a role.
On clinical presentation, 95% of patients with PsA have peripheral joint disease in the form of synovitis, tenosynovitis, dactylitis, and/or enthesitis, often asymmetric. They can have little psoriasis and terrible arthritis, or vice versa, Mixon said. They dont automatically correlate with each other. The one thing that does, though, is nail psoriasis. That will correlate with dactylitis, which is basically an inflamed sausage-like finger or toe, which happens for no apparent reason. That is a classic finding of psoriatic arthritis, a slam dunk. Its important to refer those patients to a rheumatologist.
Don’t Miss: What To Do To Relieve Upper Back Pain
What Are Drug Therapies For Psoriatic Spondylitis
Treatment of psoriatic arthritis is similar to treatment of rheumatoid arthritis when dealing with disease of the peripheral joints. The benefits of these therapies for spinal disease continue as an active topic of research. As in ankylosing spondylitis, NSAIDs decrease spine stiffness and pain. As opposed to AS patients, NSAIDs are not adequate by themselves to control skin and joint disease in the spine.
Getting Tested For Psoriatic Arthritis
Although there are no definitive tests for PsA, your dermatologist or rheumatologist can make a diagnosis based on your medical history and a physical exam, along with other factors, such as:
- signs and symptoms
- multiple screenings
- laboratory test to help rule out other conditions
If you have any of the psoriatic arthritis symptoms listed above, its important to tell your dermatologist or rheumatologist right away.
Who is treating your psoriatic arthritis? Please select one answer below.
Read Also: Can Psoriatic Arthritis Cause Lower Back Pain
Management Of Ibp And Mbp
Standard management of IBP symptoms includes patient education, the use of nonsteroidal anti-inflammatory drugs , and structured physiotherapy/exercise programs 2) . Patient education is an important aspect of IBP management, allowing patients to make informed shared decisions with their doctors . Conventional synthetic disease-modifying anti-rheumatic drugs can also be prescribed in addition to biologic DMARDs in patients with consistently high disease activity .
In 2019, the European League Against Rheumatism published updated guidelines for managing PsA with pharmacological therapies 2) . Phase 1 of treatment consists of NSAIDs with or without local glucocorticoid injections, and phase 2 treatment consists of methotrexate however, patients with predominantly axial disease directly enter phase 3 of treatment after phase 1 failure, which involves initiation of a bDMARD interleukin -17A inhibitors would be preferred over TNFis in the presence of relevant skin involvement . Because of the lack of clear efficacy in axSpA, drugs targeting the IL-12/23 pathway are not indicated for patients with predominantly axial disease .
How Is Spinal Arthritis Diagnosed
Your doctor may use some or all of the following diagnostic methods to confirm spinal arthritis:
-
Medical history and physical exam
-
Blood tests for genetic markers and/or RA antibodies
-
X-rays of the spine to locate the arthritic joint
-
MRI, CT scan, myelography, bone scan and/or ultrasound to zero in on the damage, detect nerve and spinal cord involvement or rule out other causes
-
Joint aspiration: testing of the synovial fluid inside a joint
To pinpoint the painful joint, your doctor may numb it with an injection and check whether the pain goes away.
Also Check: Does Arthritis Pain Come And Go
Recommended Reading: How Often Can You Take Aleve For Back Pain
Skin And Nail Problems
While its possible to have PsA and AS at the same time, its comparatively rare for AS patients to develop psoriasis or nail issues. Theyre much more common in PsA, reported by the vast majority of patients.
Despite these clues, identifying either disease can be complicated and may take a long time. In fact, waiting between seven and 10 years for a diagnosis is normal for people with AS. This is partly because back pain is so common and patients often wait to bring it up with a physician. Its also due to misdiagnosis many primary care doctors simply dont know much about AS, and may mistake it for a different condition like fibromyalgia.
Similarly, PsA can be misdiagnosed for rheumatoid arthritis, osteoarthritis, or gout.
Traditional Treatment Cautions Can Psoriasis Cause Lower Back Pain
You make an appointment to see your doctor because your psoriasis is flaring. He takes a look and then whips out his prescription pad to order one of the following:
. A prescription strength topical treatment
. phototherapy
. oral and injection therapy
. over the counter drugs
Any of these treatments may work fine to relieve your symptoms and make you feel better for now. The trouble with conventional treatment methods is that they rarely work to cure the underlying cause of this skin condition and that can leave you suffering repeat attacks. Still it is important to know what helps are available, and how they may help or hurt your chance of treatment success.
Topical Ointments Can Psoriasis Cause Lower Back Pain
Topical ointments are used at the first sign of psoriasis. If caught early enough they can sometimes stave off a full-blown attack. Unfortunately, most people report becoming immune to them when used often, which makes them useless for long term use. Still, using the occasional cream or gel can help relieve some of your symptoms. Steroids
Both topical and internal steroids can be prescribed to help ease psoriasis swelling inflammation and itching. Immunomodulators
An immune suppressing drug that was originally used to help transplant patients beat organ rejection, Cyclosporine helps to inhibit T lymphocyte production so that scaly plaque is unable to grow on the surface of the skin.
Oral Retinoid Can Psoriasis Cause Lower Back Pain
. stretch marks
Don’t Miss: How To Relieve Acute Lower Back Pain
What To Look Forand What To Do About It
by Health WriteriStock/ozgurdonmaz
Psoriatic arthritis doesnt always lookor feelthe same. Sometimes, symptoms are gradual and mild others might occur quickly and severely. Worsening joint pain and swelling, or new or worsening psoriatic lesions, are the most common red flags that someone is having a PsA flare, says Yamen Homsi, M.D., the section chief of rheumatology at NYU Langone Hospital in Brooklyn, NY. But there may be other signs that a flare is on the way. Knowing what to look out for is important so you can let your doctor know whats going on and stay one step ahead of a flare.
How Arthritis In The Back Is Treated

Treatment for back arthritis depends on many factors, including your age, level of pain, type and severity of arthritis, other medical conditions and medications, and personal health goals. Because joint damage caused by arthritis is irreversible, treatment usually focuses on managing pain and preventing further damage.
You May Like: What Kind Of Soap In Bed For Back Pain
Psoriatic Arthritis Can Potentially Lead To Permanent Deformity And Disability
4 minute read
When a joint pain or joint tenderness exhibits, it might be solely mistaken for arthritis a common condition that causes pain and inflammation in the joints. In fact, if swollen or tender joints are present with scaly skin patches, psoriatic arthritis might be indicated. If it is left untreated, some patients with psoriatic arthritis can further develop a severe and disabling form of arthritis. Over time, arthritis destroys the small bones, leading to permanent deformity and disability.