Who Is At Risk For Ms
While much remains undiscovered about the causes of multiple sclerosis, we have identified several risk factors, including:
- Ethnicity: Caucasians, especially of Northern European descent, have the highest risk of developing MS.
- Family history: Patients who have a parent or sibling with MS are at increased risk of developing the disease.
- Climate: MS appears to be more prevalent in temperate climates, including the northern U.S. and Canada.
- Infection: Some viral infections, including human herpes virus 6 and the Epstein-Barr virus , are associated with MS.
- Smoking: Smokers who have one MS symptom-signaling attack are more likely to have another.
- Vitamin D: Low exposure to sunlight and low vitamin D levels are associated with a greater risk of MS.
Sex Differences In Multiple Sclerosis And Associated Pain
Females are more often affected with MS than men, a phenomenon shared with several other autoimmune diseases. The prevalence and incidence of MS is two-to-three fold higher in females, compared with males . Similar sex differences were found for MS-associated pain. Whereas female MS patients experienced more severe pain than females in the general population, no difference in pain severity was found between male MS patients and men in the general population . Another study also suggested a sex difference in pain prevalence among MS patients, showing a higher female-to-male ratio among MS patients with pain compared to MS patients without pain . In contrast, some newer studies did not detect sex differences for pain prevalence in MS . Altogether, there is evidence for sex differences in MS-associated pain however, this has not been sufficiently addressed compared to the general sex differences on pain and, therefore, gender-dependent pain prevalence is still controversially discussed.
Are There Different Treatments If Your Eyelids Are Affected Because Of Covid
If you have blepharitis due to COVID-19, your doctor may recommend one of the treatments above to help manage your symptoms, such as eyelid cleansing or eye drops to reduce discomfort.
Its also likely that theyll suggest that you take general measures to care for yourself while youre ill. These include:
- getting plenty of rest
Also Check: How To Sleep When Having Lower Back Pain
Why Does Pain Occur In Ms And What Are The Common Types
Steady and achy types of pain in MS may be a result of muscles become fatigued and stretched when they are used to compensate for muscles that have been weakened by MS. People with MS may also experience more stabbing type pain which results from faulty nerve signals emanating from the nerves due to MS lesions in the brain and spinal cord.
The most common pain syndromes experienced by people with MS include:
- continuous burning pain in the extremities
- painful tonic spasms
Experts usually describe pain caused by MS as musculoskeletal, paroxysmal or chronic neurogenic.
Musculoskeletal pain can be due to muscular weakness, spasticity and imbalance. It is most often seen in the hips, legs and arms and particularly when muscles, tendons and ligaments remain immobile for some time. Back pain may occur due to improper seating or incorrect posture while walking. Contractures associated with weakness and spasticity can be painful. Muscular spasms or cramps can be severe and discomfiting. Leg spasms, for example, often occur during sleep.
Paroxysmal pains are seen in between five and ten per cent of people with MS. The most characteristic is the facial pain of trigeminal neuralgia, which usually responds to anticonvulsants such as carbamazepine, oxcarbazepine and lamotrigine.
Neurogenic pain is the most common and distressing of the pain syndromes in MS. This pain is described as constant, boring, burning or tingling intensely. It often occurs in the legs.
The Brain And Spinal Cord: Where Symptoms Typically Start
Lesions in the brain may affect cognitive abilities. Some people with MS have trouble with memory, attention and concentration, multitasking and decision-making, says Dr. Scherz. The changes are usually mild at the beginning, but can be frustrating as time goes by.
MS may also cause emotional changes, such as decreased tolerance for stress and worsening anxiety and depression, either due to nerve fiber damage or simply the burden of dealing with the disease.
Vision changes are often one of the first MS symptoms. It’s common that MS starts with an attack in the optic nerve, which sends visual information from the eye to the brain, Dr. Scherz says. This happens because the optic nerve is close to the brain, and the myelin in the eye and brain is similar, she explains. People may experience blurred vision, double vision, eye pain or loss of color vision.
Difficulty articulating words or swallowing and slurred speech may occur if theres damage to the area that controls the mouth and throat. MS may lead to a loss of sensation in whatever area of the body corresponds with the damaged area of the brain or spinal cord, Dr. Scherz says. This can cause numbness or a tingling sensationfor instance, in the fingers or toes. The feeling usually comes and goes, and can be mild or severe.
You May Like: What Causes Severe Lower Back Pain When Standing
Current And Future Developments
Next to conventional pain therapies using antidepressants and anticonvulsants, novel therapeutic approaches are currently being developed. Since MS is an inflammatory disease, most drugs used to treat MS-related motor symptoms target the inflammatory process. Interestingly, current research also identified the peripheral immune system as a relevant target for therapeutic intervention for pain. An important protein of peripheral inflammation is the mammalian target of rapamycin , which has been implicated in behavioral hypersensitivity associated with neuropathy and pain . Administration of rapamycin, an inhibitor of mTOR, not only reversed clinical signs of EAE motor disease but also ameliorated pain in EAE animals . Most likely, the therapeutic effect of rapamycin in EAE is dependent on its immunosuppressive activity involving inhibition of effector T-cells, expansion of regulatory T-cells, and inhibition of glial cell activation all processes shown to contribute to the pathology of MS-associated chronic neuropathic pain. In line with this, anti-inflammatory cytokine gene therapy reduced EAE disease course and prevented mechanical allodynia . In addition, fingolimod, an immune suppressive drug that reduces MS relapse rates and lesion frequency , has been shown to promote pain alleviation in animals with peripheral nerve injurymediated pain conditions .
Physical And Occupational Therapy
Rehabilitative therapies, such as physical therapy and occupational therapy, are important for anyone with MS not just those who have back pain. These therapies will help keep you as flexible, mobile, and active as possible. They can also teach you how to conserve your energy and move your body more efficiently.
A physical therapist can teach you exercises to help relieve some of your MS-related symptoms. They may teach you how to stretch tight muscles to alleviate your back pain. They may also recommend gait training to help you learn how to walk more easily.
An occupational therapist can teach you how to adapt your home, work, and lifestyle to meet your changing needs. They can teach you how to integrate adaptive aids into your daily habits and environments, as well as how to use them correctly. This may prevent back pain thats related to muscle strain or poor posture.
Recommended Reading: How Can I Reduce My Lower Back Pain
Treatment Of Pain In Ms
Exercise and physical therapy may help to decrease spasticity and soreness of muscles. Regular stretching exercises can help flexorspasms. Relaxation techniques such as progressive relaxation, meditation and deep breathing can contribute to the management of chronic pain.
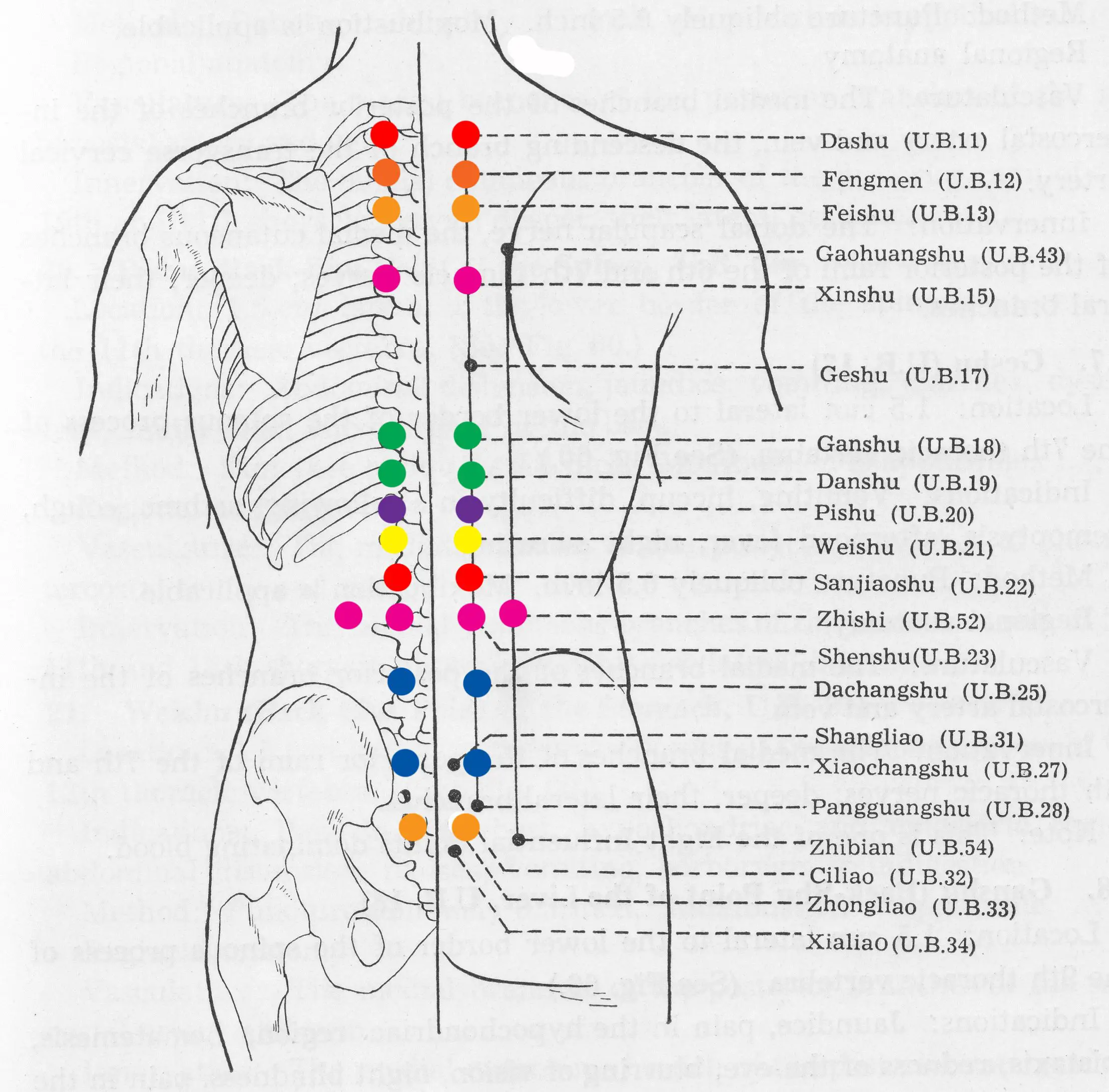
Other techniques which may relieve pain include massage, ultrasound, chiropractic treatments, hydrotherapy, acupuncture, transcutaneous nerve stimulation , moist heat and ice.
Pain from damage to the nerves in the central nervous system in MS is normally not relieved by the usual analgesics . Drugs that treat seizures and antidepressants are often effective in these cases. Treatment for spasms can include baclofen, tizanidine and ibuprofen.
Pain From Nerve Damage
Damage to the nervous system can produce pain that feels like tingling or burning. The pain can be very strong, but is usually intermittent. The most common locations for this type of pain are the face, neck and torso.
Trigeminal NeuralgiaExcruciating, sharp, shock-like pain in one side of the face, lasting seconds to minutes and often repeated may be triggered by speaking or a touch. Usually settles spontaneously by itself over several weeks.Usual medications: Carbamazepine, phenytoin and baclofen. Gabapentin may also help.
Lhermittes Sign/SymptomA brief, stabbing, shock-like sensation that runs from the back of the head down the spine, brought on by bending the neck forward. It is not always painful.Usual medications: Carbamazepine or phenytoin.Other treatments: A soft collar may limit neck movement. Most often this disorder disappears spontaneously and medical treatment is not necessary.
Can cause a sharp, knife like pain behind the eyes and difficulties with vision.Usual medications: This is treated with methylprednisolone, ibuprofen, diclofenac or naproxen.
Tonic SpasmsSudden and painful muscle contractions, producing stiffness of the whole limb, which can last up to two minutes.Usual medications: Carbamazepine, phenytoin, baclofen and clonazepam.
Read Also: How Should I Sleep For Lower Back Pain
An Autoimmune Disorder Of Another Nature
Multiple Sclerosis occurs whenfor inexplicable reasonsthe bodys immune system attacks our Central Nervous System . Although traditionally thought of as an autoimmune disease, doctors are now rethinking this concept. But why? Because autoimmune diseases usually have an identifiable, triggering antigen. In other words, we can typically discern the reason for the immune systems attack through careful medical testing.
For example, often this attack occurs in response to a mutation in the genes of a cell . In other autoimmune diseases, the introduction of a virus to the body can trigger the immune response . However, with MS, researchers cannot identify the triggering antigen that urges our T-cells to attack our Central Nervous System.
How Ms Causes Back Pain
The exposed nerves in patients with MS result in a number of side effects, many of which may contribute to spine pain. Below are some of the ways in which MS can cause spine pain:
- Muscle stiffness: Patients with MS often experience muscle stiffness. The less the muscles are used, the more uncomfortable they will be, thus creating pain in areas such as the back.
- Immobility: As MS progresses, many patients are limited in their movement. This immobility can increase muscle stiffness and is a large contributor of back pain.
- Improper use of mobility aids: It is normal for MS patients to require mobility aids such as canes or walkers to get around. If these devices are not used properly, they can tweak back muscles and lead to pain or soreness.
- Poor posture: Even MS patients who have not progressed to the point that a mobility aid is needed likely have poor posture or bad balance. This throws off the patients walk and can cause back injury or general muscle pain.
These are causes of back pain that are a direct result of MS symptoms. However, MS can also cause back pain in those patients who already suffer from a back injury or spine pain. Because the nerves are damaged, MS patients may be less likely to compensate for and tolerate back pain as well as a healthy individual.
Don’t Miss: What Does It Mean When You Have Lower Back Pain
Know The Risk Factors
MS affects more than 2.3 million people globally. Though MS is not contagious or even directly inherited, some factors may increase the risk for this disease, including the following:
Shoemaker also cites other specific factors, either alone or in combination that may contribute to the disease, which include the following:
- Certain gene variations
- Exposure to the Epstein-Barr virus
- Low vitamin D or sun exposure
Muscle And Mobility Problems
Another culprit for low back pain in MS is related to issues stemming from immobility. For instance, if a person with MS is using their cane or another mobility-assistive device improperly, low back pain may develop.
In order to compensate for an MS-related issue like a numb or tingling leg or foot, a person’s gait may be impaired, or they may distribute their weight unnaturally, which can put a strain on the lower back. Sitting in a wheelchair all day can also put excess pressure on one’s back.
You May Like: Why Do I Feel Pain In My Lower Back
How Is Ms Diagnosed
UT Southwestern follows the McDonald Criteria, along with a patients personal health history and imaging, to diagnose MS. The criteria were updated in 2017 to streamline the diagnostic process and reduce misdiagnosis. Through the criteria, a patient must meet three qualifications:
MS symptoms vary according to the degree or stage of the disease. Since we cant predict how the disease will progress, we classify the type of MS according to the course of the disease:
Earlier Diagnosis Means Better Outcomes
Knowing what signs and symptoms to look for early has tremendous benefits.
“From some of the longer duration studies, detecting MS earlier and starting MS therapies earlier tend to improve the chances of having a good long-term outcome. Patients started on MS therapies earlier in their disease tend to have a lower likelihood of reaching certain disability milestones, like needing a cane or walker,” Shoemaker says.
Although receiving an official MS diagnosis can be overwhelming, Shoemaker ensures that his patients understand how treatment can help. With nearly 15 Food and Drug Administration-approved therapies available, and new ones constantly being developed that are increasingly effective, management of MS continues to improve.
“We are at a point where we’re happy with how good we are at controlling the inflammatory aspect of the disease,” Shoemaker says. “Now we’re working on trying to improve patients’ overall quality of life so they can lead healthy, productive lives as if they don’t even have MS.”
Read Also: Can Pregnancy Cause Back Pain
Ms Can Also Look Like This
Another potential harbinger of MS is clinically isolated syndrome, or CIS, but this condition is complicated.
“CIS is kind of within the spectrum of MS. In fact, sometimes CIS is just the initial presentation of MS. And people with CIS often will go on to develop multiple sclerosis, but not always,” Shoemaker explains.
CIS is basically the first brush with MS, where neurological symptoms occur that often last 24 hours. The episode may result in one symptom or multiple, depending on scarring that occurs in one place or several places. The most common CIS symptoms include the following:
- Weakness in legs
If you’re experiencing these symptoms, it’s important to see a doctor as soon as possible. If testing doesn’t reveal a high risk for MS, CIS could signal another serious condition that needs prompt attention, including the following:
- Autoimmune conditions that cause blood vessel inflammation
- Exposure to toxic materials
- Viral infection
Ms Joint Pain Management
According to the Multiple Sclerosis Association of America, about 50 percent of people identify pain as a major symptom after being diagnosed with MS, and about 48 percent of people report experiencing chronic pain.
While everyone with MS experiences pain differently, there are some general remedies, therapies, and medications that can be used to find what is right for you.
Some everyday methods you can use to improve symptoms of joint and muscle pain include:
- positive lifestyle changes such as stopping smoking and managing your weight
In addition, many people do well with physical therapy to help manage stiffness, balance, spasticity, and spasms. A physical therapist can help pinpoint problems with weak or tight muscles that can lead to joint pain in MS.
The physical therapist can teach you stretching and strengthening exercises that will improve the joint pain. A physical therapist can also evaluate gait problems and even recommend modifications that will help you walk better and put less stress on your joints.
Recommended Reading: A Lot Of Back Pain
Looking Forward To Whats Next
Today, Sara enjoys staying busy with her favorite activities: she exercises, stays close with her family, and spends a lot of time at the soccer field with her sons. Shes really looking forward to watching her sons continue to learn and grow.
Sara is excited about the future. Shes learned quite a bit about living with relapsing MS since her diagnosis in 2005including what works best for her: I think its important for people with relapsing MS to understand that its not the end of the road. Partner with your healthcare team to make sure youre on the treatment thats right for you.
How Can You Make Sure You Get The Right Support
It is important to get pain treated. You should discuss where and how much pain you have with your healthcare provider. Your own description of the pain is the most important aspect of pain assessment. To improve your descriptions keep a pain diary and watch for pain triggers. Notice things that make your pain worse such as certain movements, fatigue, or worsening of other MS symptoms. Rate your pain on a scale of zero to 10 . As you rate the pain note any activities, time of day, where you are and whom you are with. Describe the pain and what you did about it.
If you are prescribed medications, learn their names and any side effects. Ask about the best time to take each one and what it is expected to do for you. Work with your doctor to experiment with a variety of reliable treatments, including non-medical approaches if these are appropriate. The most important thing about managing pain is to be well informed about your choices and monitored closely for potential side effects.
Be an advocate in your own pain management.
Don’t Miss: Is A Heating Pad Good For Back Pain