What Causes Ulcerative Colitis
Unfortunately the cause of ulcerative colitis is unknown, although both genetic and the environmental causes have been proposed.
Most patients with ulcerative colitis do not have anyone else in the family with ulcerative colitis. However up to 20 percent of patients with ulcerative colitis have at least one relative with either ulcerative colitis or Crohn’s disease. The genes involved in ulcerative colitis are not as well understood as in Crohn’s disease, and there are no commercially available genetic tests we currently recommend for the diagnosis of ulcerative colitis.
The increase in ulcerative colitis in some populations around the world has led some researchers to believe there may be environmental causes for ulcerative colitis. Infections and diet are among other potential environmental causes for ulcerative colitis however there is not enough information in this field to make any firm conclusions. There is still much to learn in these areas and research is ongoing to determine the cause of ulcerative colitis.
Ulcerative Colitis Symptoms You Should Never Ignore
Ulcerative colitis is an autoimmune disease in which the immune system attacks the colon and causes a range of symptoms, both in the GI tract and around the body.
Symptoms of ulcerative colitis, a type of inflammatory bowel disease , can vary widely depending on how much inflammation a person has and where the inflammation is located.
Abdominal pain and bloody diarrhea are the most common warning signs of UC, and can range from mild and intermittent to severe and chronic. The pain of UC is quite common and can significantly impact quality of life. Ulcerative colitis symptoms tend to come and go, often with extended periods of time in between flares. These are called remission periods.
The disease tends to develop gradually over time, so you might not automatically think of ulcerative colitis or IBD if you have occasional abdominal pain or digestive distress.
Ongoing inflammation along with ulcers and abscesses in the intestines are additional common causes of pain. Scarring in the lining of the intestinal tract can lead to painful obstructions. Pain may occur in different areas such as the abdomen or rectal area, depending where the inflammation is located. For example, people may experience moderate to severe pain on the left side of the abdomen if the UC affects the rectum and the lower segment of colon.
UC symptoms might ebb and flow, but they wont go away unless you see a gastroenterologist and start treatment.
Can Physical Therapy Help Lower Back Pain
Physical therapy is one of the best ways to treat lower back pain, and if your bowel problems are related to back pain, it will ease those symptoms as well. Physical therapy will help ease lower back pain and help you find relief in motion. If you are struggling with this, it is best to seek physical therapy as soon as possible. This will help prevent any need for an operation down the line. In the worst cases, if you do need surgery, our team will be by your side every step of the way helping you recover.
To learn more about the link between lower back pain and constipation, or other bowel problems, call ProFysio Physical Therapy at 812-5200 or contact us online.
Categories
Dont Miss: How To Fix A Bad Lower Back
Recommended Reading: How To Get Air Out Of Your Lower Back
How To Relieve Ulcerative Colitis Pain
While there is no cure for UC, there are ways to relieve the pain and reduce the inflammation you feel. Dietary modifications are one strategy to help manage the pain. Shifting to a low fiber, low residue diet can help you find relief. Incorporate more low fiber fruits such as bananas, non-cruciferous vegetables such asparagus, cucumbers, and carrots, refined grain products like white bread and white rice, and lean protein sources like chicken, fish, and eggs. Additionally, try to avoid consuming refined sugar, alcohol, caffeine, high fat foods, high fiber foods, and spicy foods.
Beyond nutrition, there are other ways to control the pain you feel. Focusing on managing your stress level can help. Yoga, meditation, and breathing exercises are some activities you can try on your own. Joining a support group or speaking to a mental health professional may help as well. Talking to your doctor about different medications to help control pain is also important.
Although Ulcerative colitis is life-long, that doesnt mean your UC pain has to be. When UC is well-managed, you can experience long periods of remission and become symptom-free. The key is to modify your approach based on the stage of your condition and learn to listen to your body. If youre having trouble managing your UC, we recommend working with a dietitian who can help you obtain and sustain remission.
What Kind Of Diet Is Helpful For Living With Colitis
Your healthcare provider may suggest one or several of these diets, depending on the type of colitis you have and the condition youre in:
- Low-residue diet. A low-residue diet is easy to digest when your symptoms are acute or severe. It limits fiber and fat and emphasizes soft, well-cooked foods. If you have a temporary infection or radiation colitis, your healthcare provider may recommend a low-residue diet.
- Anti-inflammatory diet. To keep chronic inflammation low, your healthcare provider might recommend you avoid highly inflammatory foods, especially fast and processed foods high in sugar and fat. They might suggest more healthy, unsaturated fats to calm inflammation like olive oil, avocados, nuts and oily fish.
- Elimination diet. If you have an inflammatory bowel disease, your healthcare provider will likely recommend an elimination diet to isolate the foods that cause your symptoms to flare up. An elimination diet eliminates certain types of foods and then adds them back in a systematic way so that you can observe how your gut responds to them. After the temporary elimination diet, you can use what you learned to design a personalized, long-term maintenance diet.
A note from Cleveland Clinic
Last reviewed by a Cleveland Clinic medical professional on 06/22/2022.
References
Recommended Reading: When Should I Go To The Hospital For Back Pain
Diagnostic Tests/lab Tests/lab Values
The diagnosis of Crohns disease is made by ruling out other potential causes to explain the patients signs and symptoms. Some of the tests include blood tests, fecal occult blood test , colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.
The blood tests are used to check for anemia which would indicate inflammation within the body, infection, and antibodies that might be present with individuals with inflammatory bowel disease.
The FOBT assesses an individuals stool sample for the presence of blood.
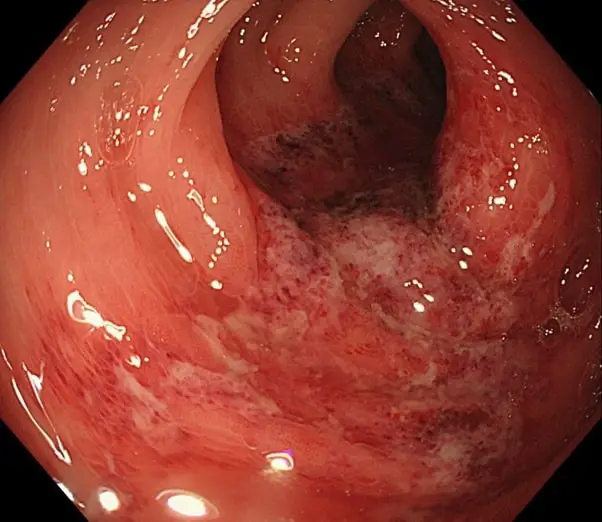
A colonoscopy allows the doctor to take a biopsy or tissue sample to determine if there is a presence of any granulomas which are common with Crohns disease and not ulcerative colitis.
The flexible sigmoidoscopy allows the doctor to assess the last portion of the colon for any biopsy samples. This allows the doctor to determine if there is any inflammation or bleeding amongst the intestines.
Barium enemas allow the doctors to assess the intestines via x-ray. The barium coats the inner lining of the GI tract to allow the lining to be visible on the x-ray.
A CT of the GI tract allows a quick look at the entire bowel in a way that cannot be seen in other diagnostic tests. This helps to assess for blockages, abscesses or fistulas.
How To Manage Joint Pain When You Have Uc
If your joints are bothering you, getting your UC under control may be the best way forward, according to Michelle Keller, Ph.D., an assistant professor in the division of general internal medicine at Cedars-Sinai Medical Center in Los Angeles. In many cases, joint pain symptoms can decrease when UC is well-managed, she says.
In fact, before exploring the severity of symptoms and treatments for joint pain, Dr. Swaminath says most gastros will zero in on asking UC patients more questions about UC treatment first. For instance, your doctor may try to determine whether your IBD is no longer in remission, or whether your disease is being undertreated. They might also ask questions to suss out whether you are having a reaction to one of your ulcerative colitis meds, which is inadvertently causing joint pain, or whether your pain is related to a separate joint problem altogether outside of your UC.
If the answers indicate the ulcerative colitis is under control but joint issues persist, it may be time to bring in the calvary, says Dr. Keller. In cases where joint pain is still present even when inflammation of the intestine is resolved, you may need to work with a gastroenterologist and a rheumatologist to identify medications that can help, she says.
Don’t Miss: Does Biofreeze Help Lower Back Pain
What Are The Complications Of Ulcerative Colitis
Colon Cancer
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
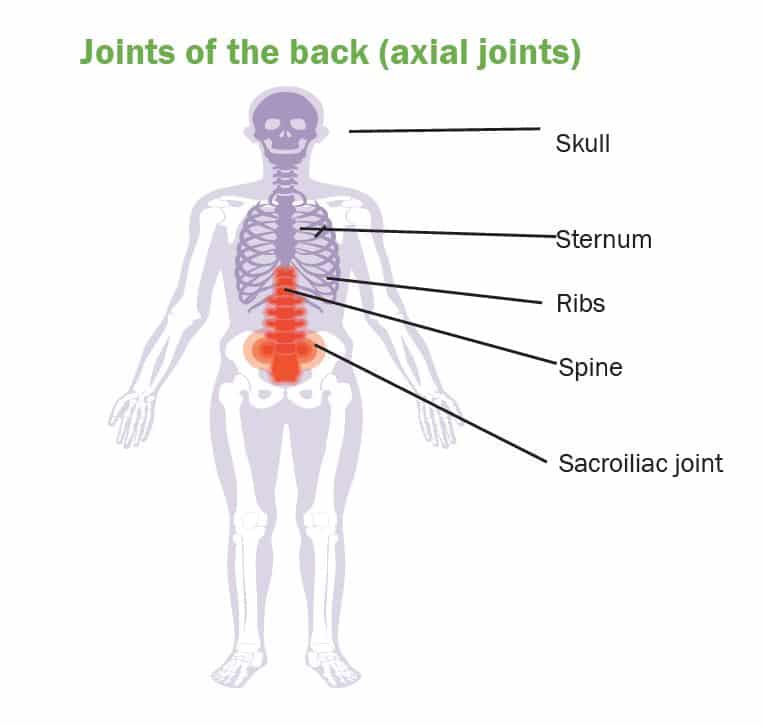
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Skin
Other Complications
Where The Pain Occurs
Pain is a common symptom of UC. According to the Crohns & Colitis Foundation, 33% of people with UC experience chronic abdominal pain. Pain management is, therefore, an important part of the treatment plan.
Pain due to UC occurs most commonly in two regions: the rectum and the lower left side of the abdomen. Doctors associate the areas of inflammation with a certain type of UC.
The severity of the symptoms can vary over time, with people often experiencing periods of mild or no symptoms, known as remission, alternating with periods of more severe symptoms, known as flare-ups.
Read Also: Do Adjustable Beds Cause Back Pain
Why Does Ulcerative Colitis Cause Joint Pain
As you can probably guess, the joint pain that occurs as a symptom of some type of Enteropathic Arthritis develops because of the inflammation caused by Ulcerative Colitis.
And no, the cause for this is yet to be found out. In normal circumstances, for some unknown reasons, inflammation occurs and affects some or more than one joint, what is later diagnosed as some type of Arthritis.
So it is not a different story this time it is still the inflammation that has first occurred because of the Ulcerative Colitis that has later only spread and affected some joints in the body, causing the common Arthritis symptoms to develop as well.
But the good news is that there are some promising suggestions for a colectomy to make the Arthritis symptoms, as well as the Ulcerative colitis symptoms, to go away.
If You Have Moderate To Severe Ulcerative Colitis
In 2020, the American Gastroenterological Association released updated treatment guidelines for adults with moderate to severe UC.
The AGA suggested that people whove never received biologics before should only receive tofacitinib if theyre a part of a clinical study or registry study.
The organization also recommended that people whove never received biologics before choose infliximab or vedolizumab instead of adalimumab .
Adalimumab isnt as effective as the other two biologics. However, people with UC can administer adalimumab to themselves, while healthcare professionals have to administer infliximab and vedolizumab. If youre looking for convenience over efficacy, its fine to choose adalimumab instead.
Don’t Miss: Does Aleve Relieve Back Pain
Basics Of Inflammatory Bowel Disease
Arthritis means inflammation of joints. Inflammation is a body process that can result in pain, swelling, warmth, redness and stiffness. Sometimes inflammation can also affect the bowel. When it does that process is called inflammatory bowel disease . IBD is actually two separate diseases: Crohn’s disease and ulcerative colitis.
Upper Middle Abdominal Pain
A type of IBD called gastroduodenal CD often causes pain in the middle and upper sections of the abdomen. These Crohns disease pain locations correlate with problems in the:
This disease type is rare, accounting for only about 4% of all diagnoses. Its even more rare for it to only impact the duodenum. This happens in just 0.07% of all CD cases.
Other symptoms of gastroduodenal CD may include:
- Fullness, or an inability to eat very much at once
| Jejunoileitis |
You May Like: Can You Eat Pizza With Ulcerative Colitis
Don’t Miss: What Could Cause Left Side Back Pain
Both Ibd And Spa Can Be Difficult To Diagnose Because The Symptoms Can Mimic Other Conditions But Correct Diagnosis Is Key To Good Care
Inflammatory bowel disease , which includes Crohns disease and ulcerative colitis, sometimes overlaps with chronic back pain, including axial spondyloarthritis an inflammatory form of arthritis. How strong this connection is, however, has been unclear, as previous studies have yielded inconsistent statistics.
In an attempt to better quantify the incidence of chronic back pain among IBD patients, researchers led by Oleg Stens, MD, at Harbor-UCLA Medical Center analyzed two massive health surveys that contained data on a total of nearly 19,000 Americans. They focused on patients who had been diagnosed with IBD and aimed to determine how many of them had experienced chronic low back pain or had official diagnoses of arthritis.
According to their findings, which were presented at the 2019 American College of Rheumatology/Association of Rheumatology Professionals Annual Meeting in Atlanta, nearly 25 percent of IBD patients had experienced chronic low back pain.
The researchers also estimated that about 10 percent of IBD patients had spondyloarthritis , which is a chronic inflammatory condition . However, they noted that proper statistical adjustments couldnt be made for SpA diagnoses since there were so few of them larger sample sizes would be needed to do that more accurately.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Also Check: How To Heal Back Pain Fast
You May Like: How Much Aleve For Back Pain
Colitis And Sacroiliac Pain Link
Spondylitis and certain types of arthritis qualify as autoimmune disorders much in the same manner as colitis. Symptoms are present because the body is actually damaging itself pathologically, rather than fending off an infection or external pathology.
Doctors are still not sure how and why autoimmune disorders occur, but there is considerable proof of a mindbody mechanism at the heart of many of these problems. Doctors know that the mind might create these syndromes much in the same manner as ischemic pain, since the conditions tend to respond well to knowledge therapy treatment, which obviously does nothing at all to change the anatomy.
The famous Dr. John E. Sarno wrote often about the relationship between autoimmune disease and what he called TMS or tension myositis syndrome. TMS is not a great diagnostic concept granted, but his work demonstrating the definitive link to the psychogenic process was nothing short of genius.
From an anatomical POV, there are chemicals in the body which cause autoimmune disorders and these are produced organically. However, while the chemistry of the diseases has been studied, doctors can not determine why the pathological change in chemistry occurs, since these particular doctors do not seek to prove the mindbody link. Instead, they are trying hard to find a purely chemical source, so that they can treat it incredibly profitably with a purely chemical solution: prescription drugs .
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Don’t Miss: What Can I Do To Help My Lower Back Pain