What Is The Link Between Arthritis And Ulcerative Colitis
When Arthritis develops as a complication of either Crohns disease or Ulcerative Colitis, usually it is one large joint on the one side of the body affected. For example, the inflammation can affect your knee on the right side and your ankle on the left side.
And according to a research published in the Journal of Clinical and Developmental Immunology, 17 to 20% of the patients with some kind of inflammatory bowel disease develop peripheral Arthritis at some point of their lives.
This type of Arthritis is also known as migratory since it begins by affecting the large joints and then it often continues by moving from one joint to another. What is most interesting is the level of inflammation of the joints that seem to be to the same extent as the inflammation of the colon caused by the Ulcerative Colitis.
Although both of these conditions cannot be entirely cured, it turns out that as soon as the symptoms of Ulcerative Colitis are managed with the proper treatment, the inflammation of the joints decreases as well. Axial arthritis, or also known as Spondylitis, also occurs, however, not so common as the peripheral Arthritis.
The symptoms of Spondylitis can develop months, even years before the Ulcerative Colitis. Affecting the lower back, Spondylitis causes great disability among these patients. And last but not least the Ankylosing spondylitis that more severe but less common among the patients with Ulcerative Colitis.
Right Or Middle Abdomen Pain
A pain that feels like cramps in the middle of the abdomen or the lower right quadrant is typical of the types of Crohn’s disease known as ileocolitis and ileitis.
Ileocolitis is the most common form of Crohn’s disease and is defined by inflammation located in the last section of the small intestine and in the large intestine .
Ileitis is a type of Crohn’s disease that affects only the ileum and is the second most common form. People with ileitis may also find that their pain or discomfort appears within a few hours of eating a meal.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Read Also: Does Acupuncture Work For Lower Back Pain
How Does Ibd Affect Pregnancy
IBD can affect your chances of getting pregnant and your symptoms during pregnancy. Pregnant women with IBD may have a high-risk pregnancy.
- Before you get pregnant: You may have more trouble getting pregnant during a flare-up . Also, if you have IBD, talk to your doctor about your risk of problems during pregnancy. If you have a flare-up during pregnancy, you have a slightly higher risk of premature birth, low birth weight, and cesarean delivery than women who do not have IBD.30
Your doctor may also change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31 If you might become pregnant, talk to your doctor about any medicines you take.
- During pregnancy: Some women say their symptoms get better during pregnancy, but others say they get worse. Women whose IBD is in remission before getting pregnant are more likely to stay symptom-free during pregnancy.31
How Is Ibd Treated
Treatments for IBD may include:
- Medicines. Most people with IBD take medicine to control their symptoms.
- Surgery. Surgery may be an option if medicine does not work to control your symptoms. Learn more about surgery for Crohn’s disease and surgery for ulcerative colitis.
- Steps you can take at home. Your doctor can talk to you about steps you can take at home to help control your symptoms and prevent flare-ups.
- Changes to your eating habits. Avoiding certain foods, changing other eating habits, and limiting or avoiding alcohol may help control your symptoms during flare-ups.
Some forms of psychotherapy, sometimes called “talk therapy,” may also help you cope with stress related to IBD symptoms and help make your pain less severe.14 Your doctor can refer you to a counselor or therapist, or you can find one at .
Some counselors specialize in working with people who have IBD. A counselor can help you talk about any distressing emotions you might have about IBD symptoms. A counselor can also treat anxiety, depression, or other mental health concerns. Ask your doctor or nurse for a referral or recommendation for a counselor in your area.
Read Also: What Helps Lower Back Pain During Pregnancy
Why Do Ovarian Cysts Develop
There are several types of ovarian cysts. Most occur as a result of a womans normal menstrual cycle, when ovarian follicles continue to grow instead of releasing eggs during ovulation. Factors that may leave a woman at an increased risk of ovarian cysts include being pregnant and having endometriosis or hormonal problems that impact ovulation.
The good news is that most ovarian cysts go away on their own. In fact, many ovarian cysts come and go without causing any noticeable symptoms. In symptomatic cases, self-care measures like using a heating pad to soothe lower back pain and taking a relaxing Epsom salt bath can help relieve any discomfort.
Can Ulcerative Colitis Cause Nausea
People may experience mild to severe nausea as a symptom of ulcerative colitis. Changing dietary and eating habits can help manage nausea. There are also medications doctors can recommend to ease feelings of nausea. Alternative therapies, such as medical cannabis, may also help.
In some cases, severe nausea may cause vomiting or loss of appetite, which may lead to malnourishment, fatigue, and weight loss.
In this article, we will look at the link between ulcerative colitis and nausea. We will also list different types of treatment that might help a person manage nausea and other related symptoms.
Ulcerative colitis can cause nausea. People may also experience vomiting, fatigue, loss of appetite, and weight loss. Symptoms can vary between people and can depend on the severity and location of inflammation in the body.
According to the National Institute of Diabetes and Digestive and Kidney Diseases , people are more likely to experience nausea and vomiting if they have severe ulcerative colitis or if the condition involves more of the large intestine.
However, a stricture may also cause nausea, along with vomiting and constipation. A stricture happens when scar tissue builds up and narrows the intestine, causing a blockage.
Read Also: How Does Chiropractic Help Back Pain
Inflammatory Bowel Disease Treatment
The goal of treatment is to get rid of the inflammation that causes your symptoms. Many types of medicine can help reduce inflammation. Talk to your doctor about anti-inflammatory drugs and drugs that suppress the immune system. Some medicines are needed only during flare-ups. You may need long-term medicines to suppress your immune system. Depending on your symptoms, your doctor may also recommend these medicines and supplements:
- Antibiotic
- Pain reliever
- Vitamin supplements
In severe cases of inflammatory bowel disease, you may need to go to the hospital for intravenous fluids or surgery.
During your treatment, you will most likely be treated by a team of doctors. This team may include your family physician, a gastroenterologist , and, possibly, a surgeon.
Diagnostic Tests/lab Tests/lab Values
The diagnosis of Crohns disease is made by ruling out other potential causes to explain the patients signs and symptoms. Some of the tests include blood tests, fecal occult blood test , colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.
The blood tests are used to check for anemia which would indicate inflammation within the body, infection, and antibodies that might be present with individuals with inflammatory bowel disease.
The FOBT assesses an individuals stool sample for the presence of blood.
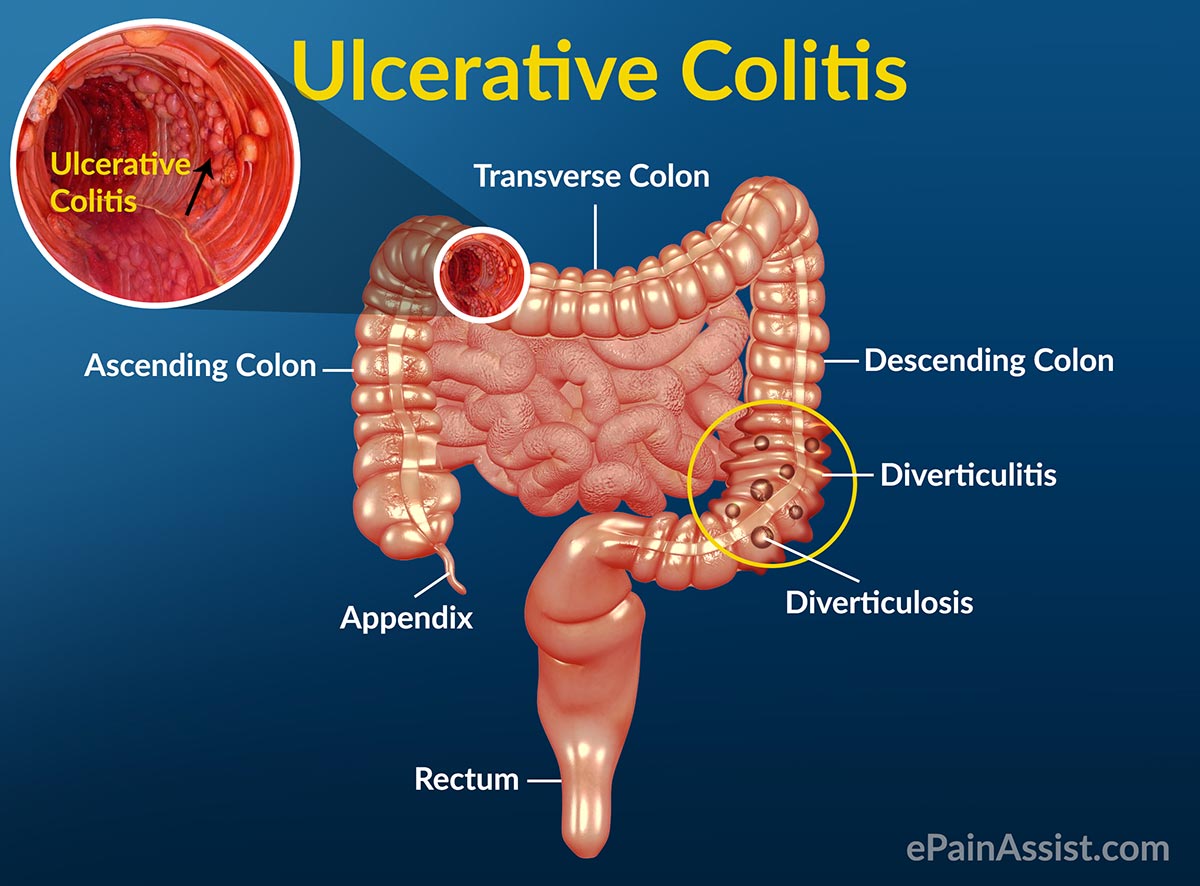
A colonoscopy allows the doctor to take a biopsy or tissue sample to determine if there is a presence of any granulomas which are common with Crohns disease and not ulcerative colitis.
The flexible sigmoidoscopy allows the doctor to assess the last portion of the colon for any biopsy samples. This allows the doctor to determine if there is any inflammation or bleeding amongst the intestines.
Barium enemas allow the doctors to assess the intestines via x-ray. The barium coats the inner lining of the GI tract to allow the lining to be visible on the x-ray.
A CT of the GI tract allows a quick look at the entire bowel in a way that cannot be seen in other diagnostic tests. This helps to assess for blockages, abscesses or fistulas.
Recommended Reading: How To Stretch Lower Back Muscles Pain
Routine Screening To The Rescue
When the physician turned 60, he scheduled a colonoscopy, a recommended test to screen asymptomatic individuals over 50 for colon cancer. He had one at 50 it was completely normal. When it was time for his next exam, the doctor who did it the first time had retired, so he asked a friend, Dr. Erick Chan, a gastroenterologist, to perform the test.
He was still a little foggy from the anesthesia when Chan came by with what the physician assumed would be the usual report of normal results. He was wrong. I took some biopsies, and well wait to see what they show, Chan said. But I have to tell you, it didnt look normal. The test had been routine until Chan got close to the spot where the colon and the small intestine connect, a structure known as the ileocecal valve. Chan noticed that the valve looked a little asymmetric.
As Chan advanced his scope, he could see that the valve was distorted by scar tissue so much so that the connection was too narrow for his instrument to enter. Bringing his scope as close to the opening as he could, he saw that the tissue on the other side was an angry red and dotted with ulcers. They would have to wait for the biopsies to come back, but Chan suspected Crohns disease. Thats impossible, the man responded. He had no G.I. symptoms at all. No pain, no diarrhea, no blood in his stools. How could he possibly have Crohns?
Complications Of Ulcerative Colitis And How To Avoid Them
Learn how to identify and avoid potentially life-threatening complications of ulcerative colitis.
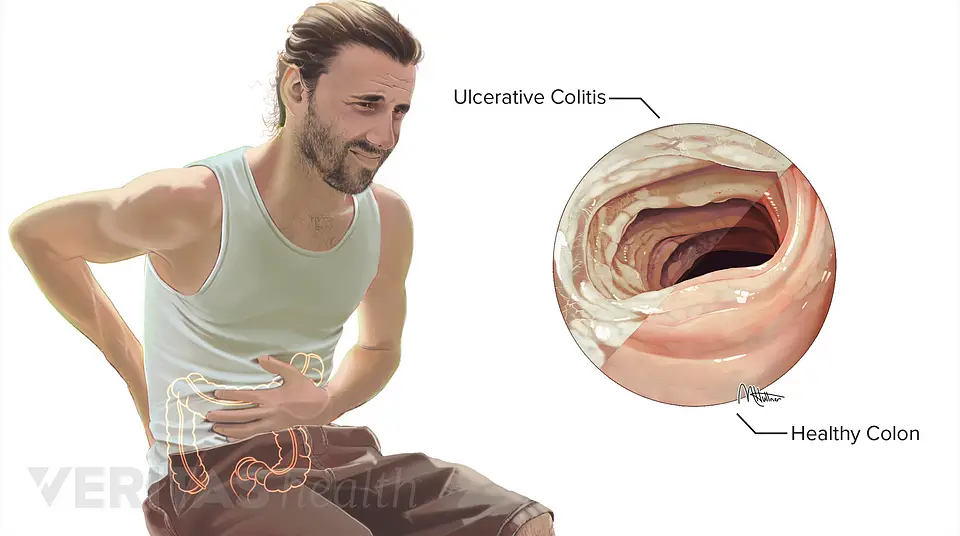
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
“It’s easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,” says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
Also Check: How To Reduce Back Pain
When Should You Call Your Doctor
If youre experiencing certain symptoms, chances are, your current treatment is not working and its time to consider a change in therapy, says Ha. Call your doctor if:
- Cramping is severe
- Youre experiencing a significant amount of abdominal pain that requires medication
- You have a fever that lasts longer than a couple of days
- You experience nausea or vomiting
- You have ongoing diarrhea or blood in your stool
How Is Abdominal Pain With Ibd Diagnosed
If your abdominal pain and cramps get worse, it could be a sign that your inflammatory bowel disease is flaring up.9 It may be necessary to see your health care provider.
You may need blood or stool tests to check for signs of inflammation. Your provider may want to do procedures such as colonoscopy or upper endoscopy, computed tomography scan, or small-bowel follow-through. These procedures are done to check for inflammation, obstruction, or abscess.9
Recommended Reading: Are Epidural Injections For Back Pain Safe
What Causes Back Pain In Ulcerative Colitis
- Fatigue
- Weight loss
A person having backaches may not realize its related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
Poor Growth And Development
Ulcerative colitis, and some of the treatments for it, can affect growth and delay puberty.
Children and young people with ulcerative colitis should have their height and body weight measured regularly by healthcare professionals.
This should be checked against average measurements for their age.
These checks should be carried out every 3 to 12 months, depending on the person’s age, the treatment they’re having and the severity of their symptoms.
If there are problems with your child’s growth or development, they may be referred to a paediatrician .
Don’t Miss: How To Prevent Back Pain From Standing All Day
Episcleritis: Uncomfortable But Not Worrisome
This condition is one of the most common associated with UC and IBD, says Dr. Shah. Episcleritis is inflammation of the episclera, which is the connective tissue between the sclera and the conjunctiva . This condition can cause redness, pain, and tenderness in the eyes, Dr. Shah explains, adding that you may also feel the sensation that something is in your eye. Your doctor may prescribe steroid eye drops, but episcleritis often resolves on its own in a few weeks.
Prevalence Of Pain In Ibd
A total of 1263 completed questionnaires was analyzed regarding pain. The vast majority of patients reported having experienced pain in general during the course of the disease. Only 369 of the patients that sent back the questionnaire reported no pain . There was no statistical difference when comparing CD and UC regarding the occurrence of pain . When comparing the prevalence of pain in patients with any extraintestinal manifestation and without, slightly more patients with EIM reported pain, but this did not reach statistical significance .
Also Check: Do Chiropractors Help With Lower Back Pain
When To Contact A Doctor
A person living with UC should talk with their doctor if they notice symptoms associated with sacroiliitis, such as pain in the hips when walking or any other types of arthritis. A primary care physician may refer a person to a rheumatologist for diagnosis.
A person may want to consider a second opinion if their doctor does not refer them to a rheumatologist. Early referrals can help improve treatment outcomes. However, referral rates are low, according to a 2018 study .
If symptoms get worse during treatment or do not improve, a person should talk with a healthcare professional. A doctor can recommend additional therapies that may help improve symptoms of either UC or sacroiliitis.
As a person begins to better manage their UC symptoms, they will often notice an improvement in their sacroiliitis symptoms, too.
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Recommended Reading: Why Is My Lower Back And Hip Hurting
What Is Uc Cramping
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.