What Causes Rectal Prolapse
- Anything that increases the pressure inside your tummy can make you more likely to develop a rectal prolapse. This can include:
- Straining to pass urine due to a swollen prostate gland.
- Damage to the back passage or pelvis from previous surgery.
- Damage to the muscle on the floor of the pelvis.
- Infections of the bowel with certain types of microbes called parasites .
- Diseases of the nervous system such as multiple sclerosis.
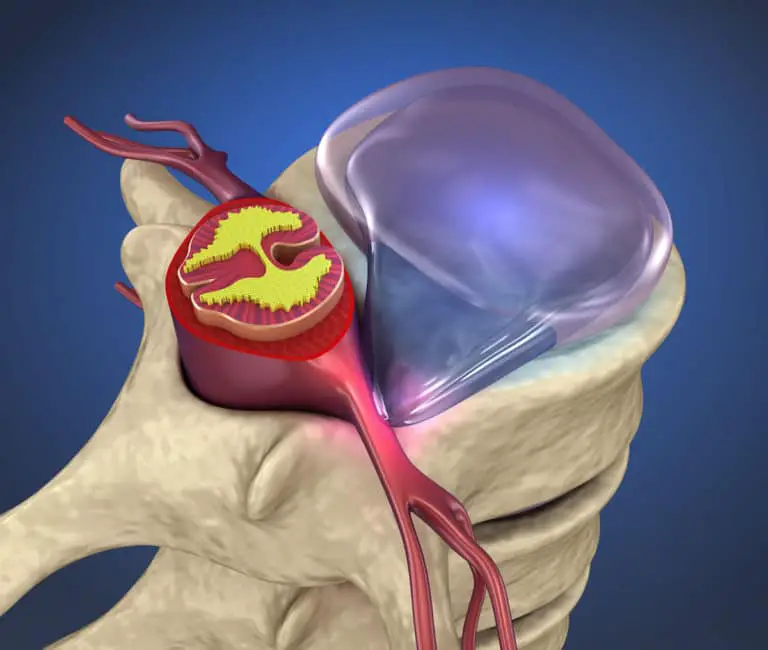
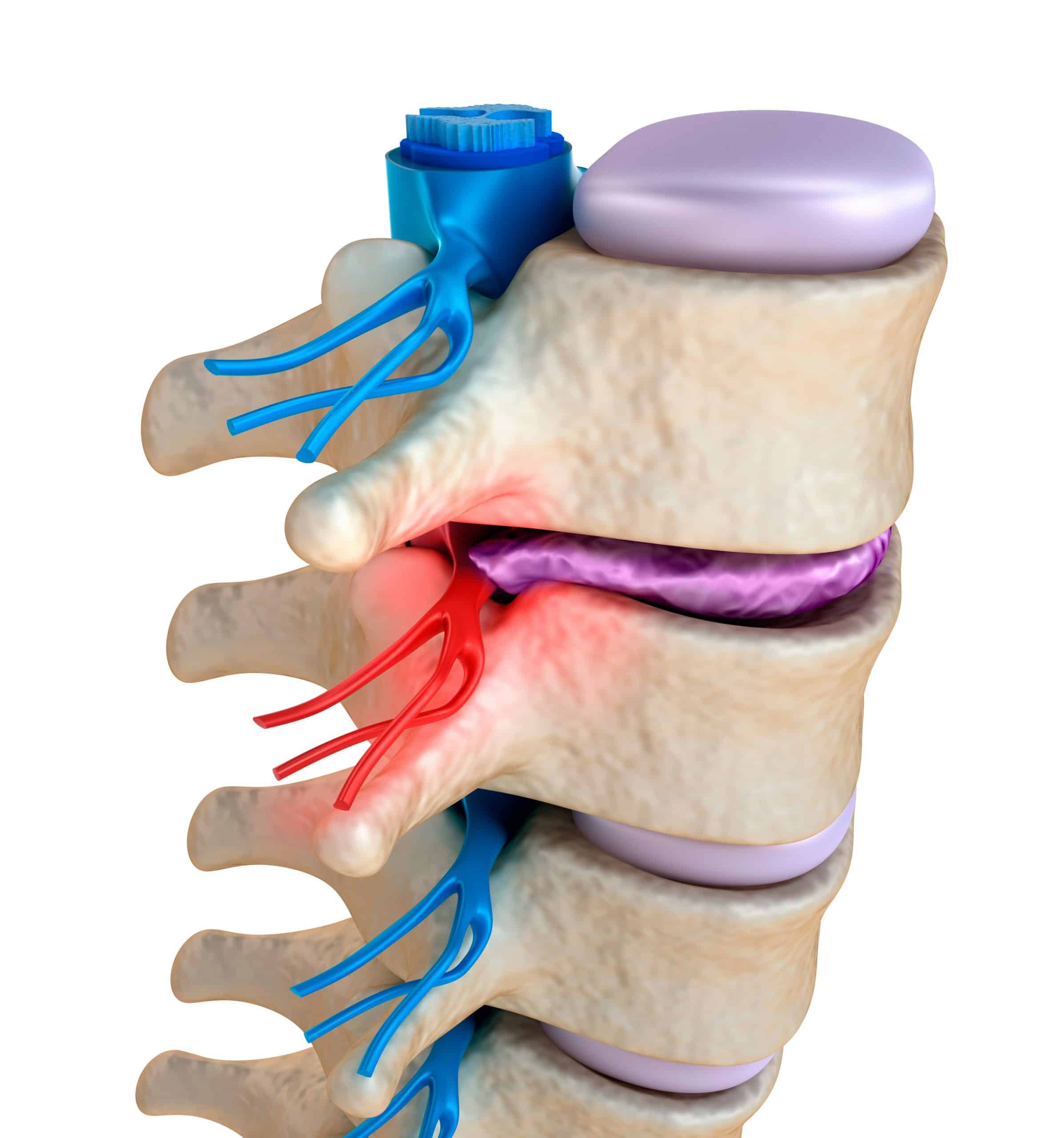
- Damage to the nerves from back surgery, a slipped disc, or an accident injuring the pelvic nerves.
- Mental health conditions associated with constipation, such as:
- A side-effect of medicines used to treat psychiatric disorders.
In children, rectal prolapse can occur in:
- Hirschsprungs disease .
Prolapse of the bladder or womb doesnt cause rectal prolapse but is sometimes associated with it.
Treatment Of Pelvic Organ Prolapse
Treatment of pelvic organ prolapse is based on the woman’s symptoms. Treatment aims to improve quality of life.
Doctors start by closely monitoring the woman and her symptoms.
If symptoms are bothersome, treatment may include pelvic floor exercises, a pessary, and, if symptoms are severe, surgery. If women do not have symptoms or symptoms are mild, no treatment is needed. However, follow-up visits are needed to monitor the progression of the prolapse.
How Can I Reduce My Risk Of Uterine Prolapse
Some factors like having multiple vaginal births or experiencing menopause cant be avoided.
There are ways to reduce your risk of developing a prolapse. A few lifestyle tips that can reduce your risk of prolapse include:
- Maintain a healthy weight and exercise regularly.
- Do Kegel exercises to strengthen your pelvic floor muscles.
- Stop smoking. This reduces the risk of developing a chronic cough, which can put extra strain on your pelvic muscles.
- Using proper lifting techniques when carrying heavy objects.
- Avoid becoming constipated or straining to poop.
Proper lifting techniques to avoid uterine prolapse
There are several tips for lifting heavy objects that can help you avoid injury, including:
Recommended Reading: How To Stop Chronic Back Pain
Is Pelvic Floor Dysfunction Related To Interstitial Cystitis
Interstitial cystitis is a chronic bladder condition that causes pain in your pelvis or bladder. Pain from the bladder can cause pain in the pelvic floor muscles and then loss of muscle relaxation and strength which is pelvic floor dysfunction. So, having one of these conditions increases your risk of having the other.
If youre taking certain medications for interstitial cystitis, including antidepressants, these might cause constipation. Constipation can lead to worsening of your pelvic floor dysfunction symptoms. Check with your provider in case your prescription might be causing this problem.
Pelvic Floor Weakness Impacts More Than You Think
by Tiffany Regdos | Oct 4, 2016 | Low Back, Women’s Health
Help a Friend:
Urinary incontinence affects over 50% of postmenpasual women, 30% of women post partum, and 3-5% of women in high level sports . With so many women affected, why is there still a stigma surrounding this topic? Difficulty controlling your bladder or leakage of urine upon exertion is something that women can experience due to a weak pelvic floor. However, the pelvic floor does more for your body than simply control your bladder. Pelvic floor dysfunction can lead to back pain, sacroiliac dysfunction, and even hip pain. If you have had low back pain or sacroiliac pain and have tried multiple therapies without relief you may want to strengthen this often overlooked culprit.
The pelvic floor muscles attach from your pubic bone to your tail bone and act as a supportive sling for your bladder, uterus, and rectum. The pelvic floor becomes active when you exert a downward force on it by contracting your abdominals and diaphragm. Certain activities will increase the amount of force required from the pelvic floor. Major increases occur from coughing, sneezing, laughing, running, and jumping . I know what you are thinking, How does this relate to my back pain?
Recommended Reading: What Could Cause Severe Lower Back Pain
Back Pain And Bladder Cancer
Pain in the lower back and/or abdomen can sometimes be caused by bladder cancer, and it is more common in patients who are diagnosed with bladder cancer that is advanced or metastatic. The symptom is not usually experienced by patients who are diagnosed with bladder cancer that is considered early stage. The most common symptom of bladder cancer is blood in the urine that is visible to the eye, which is experienced by around 80% to 90% of patients diagnosed. Between 20% and 30% of patients diagnosed with bladder cancer experience other problems or changes related to urination, such as
- The need to urinate more frequently than usual
- Pain or burning before, during or after urination
- Feeling the urgent need to urinate despite the bladder not being full
- Being unable to urinate
If you experience lower back or abdominal pain as well as any of those symptoms related to urinationand especially if you have ever noticed blood in your urine then you should let your healthcare provider know. If the symptoms are being caused by bladder cancer, then finding it out as soon as possible is important so you can begin treatment.
Can Uterine Prolapse Be Prevented
There is no certain way to prevent uterine prolapse. However, the following can help lower your risk:
-
Lose weight, if youre overweight
-
Follow a diet rich in fiber and fluids to prevent constipation and straining
-
Avoid heavy lifting
-
Quit smoking, if you smoke
-
Seek prompt treatment for a chronic cough, which can place extra pressure on your pelvic organs
-
Do Kegel exercises to strengthen your pelvic floor muscles
These actions may also help if you already have uterine prolapse.
See your healthcare provider when symptoms first start to bother you. Dont wait until your discomfort becomes severe. Regular pelvic exams can help detect uterine prolapse in its early stages.
Also Check: What Weed Is Good For Back Pain
How Do I Know If Pelvic Floor Dysfunction Is Causing My Low Back Pain
First of all, it’s extremely likely that pelvic floor dysfunction is at least contributing to back pain symptoms that won’t go away. In one study of chronic low back pain, 95% of people also had pelvic floor dysfunction! They had been getting treatment for years – orthopedic physical therapy, chiropracters, acupuncture, and even surgery – without results!
Because they weren’t getting to the underlying “why” of what was going on for lasting relief!
Other research has tied low back pain to urinary incontinence, with nearly 80% of women with chronic back pain reporting at least occasional incontinence.
What Is The Link Between Pelvic Floor And Back Pain
- Posted 19 June 2019
- Feeling good in my body
The back is subject to constraints during the day because of activities of daily life but also during the night because of the lying position maintained for several hours. Although the back generally appreciates movement and dislikes immobility, not all movements are good for it. Lower back pain can have many causes that are often misdiagnosed. A weakened pelvic floor can also be related to back pain. So if you have any doubts, consult your doctor.
Here are the main ones:
Don’t Miss: What To Take For Lower Back Spasms
Treatment For Pelvic Organ Prolapse
If you do not have any symptoms, or the prolapse is mild and not bothering you, you may not need medical treatment.
But making some lifestyle changes will probably still help.
These include:
- losing weight if youre overweight
- avoiding heavy lifting
- preventing or treating constipation
If the prolapse is more severe or your symptoms are affecting your daily life, there are several further treatment options to consider.
These include:
- vaginal pessaries
The recommended treatment will depend on the type and severity of the prolapse, your symptoms and your overall health.
You and your doctor will decide together whats the best option for you.
Does Ice Help Lower Back Pain Low Back Pain Bloated Abdomen Nausea
Best Weight Exercise For Lower Back Pain Lower Back Pain Hyrst When I Stand Up But Then Goes Away Does Prolapsed Bladder Cause Low Back An Pain In Stomach. Stretch Middle Back Pain Sharp Breath Taking Pain In Mid Back Left Side What Do I Do. Chronic Knees And Back Pain Sleep Apnea Cause Me To Stay In Bed Chronic Back Pain Recovery Stories. Pain In Upper Back When I Bend Over Pain Shoots To Butt Locate Upper Back Pain Chart.
Too Much Walking Lower Back Pain Lower Back Pain Is Excruciating. Is A Recliner Good For Lower Back Pain Yoga Exercises For Upper Back Pain Relief Explain Chronic Back Pain To Patients. Looking Down And Feeling Pain In Lower Back Upper Back Pain Woorsed By Swallowing.
Also Check: Why Is My Bladder Always Full
Recommended Reading: What Causes Lower Back Hip And Knee Pain
How Is Uterine Prolapse Diagnosed
If your healthcare provider thinks that you have a prolapsed uterus, he or she will probably do a physical exam to check your pelvis. If you also have urinary incontinence or a feel like you cant empty your bladder, your doctor may do a procedure called a cystoscopy to examine your bladder and urethra.
Your healthcare provider might also order an MRI . This procedure uses a magnet and radio waves to create images. This will allow your healthcare provider to get a good look at your kidneys and other pelvic organs.
How Do You Fix A Prolapsed Uterus
There are surgical and nonsurgical options for treating uterine prolapse. Your healthcare provider will pick your treatment path based on the severity of your prolapse, your general health, age and whether or not you want children in the future. Treatment is generally effective for most people. Treatment options can include:
Nonsurgical options
- Exercise: Special exercises, called Kegel exercises, can help strengthen your pelvic floor muscles. This may be the only treatment needed in mild cases of uterine prolapse. To do Kegel exercises, tighten your pelvic muscles as if youre trying to hold back urine. Hold the muscles tight for a few seconds and then release. Repeat 10 times. You may do these exercises anywhere and at any time .
- Vaginal pessary: A pessary is a rubber or plastic doughnut-shaped device that fits around or under the lower part of your uterus . This device helps prop up your uterus and hold it in place. A healthcare provider will fit and insert the pessary, which must be cleaned frequently and removed before sex.
- Diet and lifestyle: Changes to your diet and lifestyle may be helpful in relieving symptoms like constipation. Increasing your water and fiber intake may lessen how often you strain to poop. Maintaining a healthy weight for your body type puts less pressure on your pelvic muscles when you stand or walk.
Surgical options
You May Like: How To Get Rid Of Back Pain While Sleeping
What Is Pelvic Floor Dysfunction
Pelvic floor dysfunction is a common condition where youre unable to correctly relax and coordinate the muscles in your pelvic floor to urinate or to have a bowel movement. If youre a woman, you may also feel pain during sex, and if youre a man you may have problems having or keeping an erection . Your pelvic floor is a group of muscles found in the floor of your pelvis .
If you think of the pelvis as being the home to organs like the bladder, uterus and rectum, the pelvic floor muscles are the homes foundation. These muscles act as the support structure keeping everything in place within your body. Your pelvic floor muscles add support to several of your organs by wrapping around your pelvic bone. Some of these muscles add more stability by forming a sling around the rectum.
The pelvic organs include:
Normally, youre able to go to the bathroom with no problem because your body tightens and relaxes its pelvic floor muscles. This is just like any other muscular action, like tightening your biceps when you lift a heavy box or clenching your fist.
But if you have pelvic floor dysfunction, your body keeps tightening these muscles instead of relaxing them like it should. This tension means you may have:
- Trouble evacuating a bowel movement.
- An incomplete bowel movement.
- Urine or stool that leaks.
Pelvic floor muscles
Its All About The Core
When you think of a strong core, do six pack abs come to mind? Our core is made of a host of muscles with the pelvic floor playing a major supportive role. The pelvic floor muscles are the base of the core. Our abdominals, low back muscles, hip muscles, diaphragm, and pelvic floor work together to stabilize the spine. The core stabilizes the spine through IAP or intra-abdominal pressure. This occurs when the diaphragm contracts down causing the pelvic floor and transverse abdominus to lift up, creating a stable environment for the spine .
As shown by the orange arrows, the muscles of the core co-contract creating stability for the spine. If the pelvic floor is weak, the pressure created by the abdominals and diaphragm exits through the pelvic floor. Without a strong base, the integrity of the lumbar spine and SI joint is comprised and can lead to injury or dysfunction . Meaning, if you have frequent urine leakage, you may be at an increased risk for developing back pain.
Still not convinced the pelvic floor does more than just control your bladder? Weakness in the pelvic floor has been linked with arthritis in the hip joint. Multiple hip muscles attach into the pelvic floor to increase the tension of the pelvic floor. Weak hip muscles due to arthritis can therefore decrease tension in the pelvic floor and contribute to incontinence issues . One study found that 64% of women with symptoms of incontinence had improvement in their symptoms after a hip replacement .
Recommended Reading: What Is Back Pain Caused By
Can Uterine Prolapse Cause Pain In Back And Leg Heaviness
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Incomplete Voiding Of The Bladder
A prolapsed bladder may press down on the tissue and nerves, making it difficult to completely empty the bladder. Some individuals with incomplete voiding of the bladder may have to urinate more than once to empty their bladder, which may require repeated trips to the bathroom. Individuals often report feeling as if they have not emptied completely, even after what they believe is full urination. This problem often leads to interruption of their everyday activities at work or school, which can lead to embarrassment. Individuals who have problems urinating should have a frank discussion with their doctor, who can point them to the appropriate specialist. It may be a prolapsed bladder.
Also Check: How To Stretch A Pinched Nerve In Lower Back
Tests For Bladder Prolapse
Tests that may be carried out to confirm or reject a diagnosis of bladder prolapse, depending on your symptoms, are:
- pelvic ultrasound to exclude any masses or cysts putting pressure on the bladder
- urodynamics a test of bladder function and to assess different types of incontinence
- a bladder scan to measure residual urine urine left in the bladder after emptying
- a midstream urine test to exclude urinary tract infection
- magnetic resonance imaging in some cases.
You May Like: Antibiotics Given For Bladder Infection
Is Pelvic Floor Dysfunction A Disability
Pelvic floor dysfunction isnt currently listed as a social security disability. However, depending on your symptoms you may be able to claim disability under the Disability Evaluation Under Social Security Section 6.00, Genitourinary Disorders. For more information, check with your provider and social security contact.
Read Also: What Kind Of Bed Is Good For Lower Back Pain
Conditions That Can Cause Pelvic Prolapse
Dr. Jones: So what conditions can cause this? We mentioned having births and we mentioned being a paratrooper.
The biggest risk factor is childbirth, then just getting older.
Dr. Jones: Oh, great.
Because, unfortunately, the longer you’re alive, the more and more gravity has its effect.
Dr. Jones: Gravity wins. Gravity always wins.
Gravity always wins, but obesity, menopause, family history, race . . . Latinas and white women are more likely to get prolapse, and a previous hysterectomy also seem to play a role in the development of prolapse.
Treatment For Bladder Prolapse
Treatment for bladder prolapse depends on how bothersome the prolapse is and its stage. The more advanced the prolapse, the more likely it is to be bothersome. During your consultation, you and your gynaecologist will discuss the most bothersome aspects of the symptoms and how they are affecting your life. A treatment plan can be tailored based on the severity of symptoms and stage of prolapse.
Read Also: Why Do You Get Lower Back Pain On Your Period
How Is Prolapse Treated
Many women with prolapse don’t need treatment, as the problem doesn’t seriously interfere with their normal activities.
Lifestyle changes such as weight loss and pelvic floor exercises are usually recommended in mild cases.
Surgery may also be an option for some women. This usually involves giving support to the prolapsed organ. In some cases, complete removal of the womb is required, especially if the womb has prolapsed out.
Most women experience a better quality of life after surgery, but there’s a risk of problems remaining or even getting worse.
Is Your Back Pain Connected To Your Pelvic Floor
by Lauren Sutherland | Aug 25, 2020 | Pelvic Health
Could your persistent low back pain be connected to your pelvic floor?
Do you suffer from low back pain that does not seem to go away despite your efforts to find relief?
According to the National Institutes of Health , more than 31 million people suffer from chronic lower back pain, and about 80 percent of all adults experience lower back pain at some point in their lifetime. About 25 percent of adult women suffer with pelvic floor dysfunction issues such as incontinence, pelvic organ prolapse, and pelvic pain. As women age, this ratio increases. Recent research has also shown that of women with low back pain more than 95% had pelvic floor dysfunction as well. This included pelvic tenderness , weakness and even pelvic organ prolapse . Other research has tied low back pain to urinary incontinence, with nearly 80% of women with chronic back pain reporting at least occasional incontinence.
Back pain and pelvic floor dysfunction are so closely related because all the muscles that support the pelvic floor must also work to support and protect the spine. When the back is in pain, the pelvic floor muscles may tighten to try and protect the sensitive area. This can overwork the pelvic floor, causing tender points, tightness, and muscular fatigue.
Read Also: Can Humira Cause Back Pain