Technical Reasons For Failure
Technical failure is likely the single largest cause of early stent failure. In the majority of cases, failure is due to inadequate treatment of inflow by not extending the stent caudally enough to manage disease in the CFV or not extending the stents cranially enough to treat outflow disease . There are several consistent bony landmarks for ensuring that stents are placed correctly.
Figure 2. Images of a patient undergoing reintervention after referral for an occluded stent. Panel A shows the line of the spinous process. The stent is short of the spinous processes and has therefore not extended cranially enough and has not stented beyond the May-Thurner/Cockett pinch point. Panel B shows the stent extended into the femoral vein beyond the confluence of the patent profunda vein. The lesser trochanter serves as a reliable landmark for the typical confluence point.
Fracture
Stent fracture may complicate extension of the stents beyond the inguinal ligament into the CFV. Typical fractures are approximately 1 cm beyond the line of the ligament and correspond to the head of the femur. Many hypotheses have been suggested regarding the cause of fracture, including compression by the ligament or against the bony prominence of the pubis. More work is needed to define this, and fracture will undoubtedly remain an issue. However, not all fractures cause clinical problems, and some may be totally asymptomatic.
Migration
Back Pain
How Can I Reduce My Risk Of May
Theres no way to prevent May-Thurner syndrome because experts dont know what causes it. But you can improve your circulation and decrease your risk of blood clots by:
- Avoiding prolonged periods of sitting.
- Drinking plenty of water.
- Exercising regularly, focusing on aerobic exercise for cardiovascular health.
- Sudden chest pain that worsens when you inhale.
May Thurner Syndrome And Back Pain
The most common symptoms are pain in the back, neck, shoulders, arms, and legs. These symptoms may be accompanied by weakness, numbness, tingling, or weakness in one or more of these areas. In some cases, the pain can be so severe that it interferes with daily activities, such as driving a car or operating heavy machinery.
The symptoms can also be severe enough that they interfere with a persons ability to work or care for themselves or their family members. Some people may experience a variety of symptoms, including: Back pain that is severe and lasts for a long period of time. This pain is often described as pins and needles pain. It may last from a few days to several weeks.
Pain that cant be relieved by rest or pain medications. People with this type of pain often have to use a cane or walk with crutches to get around. They may have a hard time lifting heavy objects or performing other activities that require the use of their legs or arms.
Recommended Reading: Why Does My Lower Back Hurt When I Look Down
What Causes Back Pain May
Back pain causes are as diverse as they are common. The most common are muscular, skeletal, and disc problems. Despite their seemingly simple nature, these conditions can be very painful. Some of the most common cause of back pain is improper posture. You should always strive to sit with your shoulders over your hips. This helps to keep your spine in the proper alignment. When you deviate from this position, you put extra pressure on your back muscles, which may lead to muscle spasms and even a spinal stenosis.
Some of the most common back pain causes are as described above: a dull ache in the back that can radiate to the buttocks or legs. Although not all cases of back pain are as serious, there are a variety of symptoms that can be caused by back issues. A doctor can determine the exact cause of your back pain by asking about your symptoms and performing a physical exam. Sometimes an x-ray will be taken to check whether your bones are aligned properly and to rule out any broken bones. Unfortunately, x-rays cant detect if your disks and nerves have been damaged.
Hematologic Reasons For Failure
Anticoagulation strategies are vital after stent placement to reduce the risk of early stent thrombosis. This is especially important in the context of acute and chronic postthrombotic disease. Although the importance of anticoagulation is reduced in patients with nonthrombotic iliac vein lesions, early stent thrombosis has still been reported, and thus it cannot be totally ignored. Animal studies have indicated that it takes approximately 56 days for the newly placed stents to epithelialize, and the data on stent thrombosis support that the risk of thrombosis is higher in the first 6 weeks after stent placement, although it may still occur later.5
In our practice, we place all patients on 2 weeks of low-molecular-weight heparin after stent placementa full treatment given as a twice daily dose. This is designed to flatten the dosing and prevent extreme troughs. After 2 weeks, we convert patients to warfarin for the first 6 months and then consider a direct oral anticoagulant if longer-term anticoagulation is needed.
We have observed no difference in outcomes between patients with or without a defined thrombophilia however, this is only achieved if the anticoagulation strategies are closely followed.
A multidisciplinary team including a hematologist with an interest in thrombosis is a vital component of managing complex patients.
Read Also: What Is The Reason For Back Neck Pain
What Questions Should I Ask My Healthcare Provider
If you have May-Thurner syndrome or think you could, you may want to ask your healthcare provider:
- What are the symptoms of May-Thurner syndrome?
- What is the most likely cause of my symptoms?
- What tests do I need to diagnose May-Thurner syndrome?
- What are the symptoms of DVT?
- What are the symptoms of a pulmonary embolism?
- What treatment do you recommend for May-Thurner syndrome?
- What are the chances that symptoms will return after May-Thurner syndrome treatment?
May Thurner Syndrome And Back Pain: Symptoms
Typically, symptoms of May Thurner Syndrome begin as mild which are worse in the left leg.
Symptoms may include fatigue, body aches, and swelling in the leg. Pelvic pain, groin pain, and lower back pain, more noticeable on the left side may also be present.
Without treatment, May Thurner Syndrome can progress and may cause long-term symptoms difficulties, and disabilities.
Read Also: How To Lose Weight With Chronic Back Pain
Can I Get May
Treatment for May-Thurner syndrome is intended to make it easier for blood to flow through the iliac vein. None of our current treatment options can eliminate the factors involved in vein compression, but some do “open” the vein using a stent. Treatment is successful in most cases and does not need to be repeated. However, there is a small chance that the compression that caused symptoms could recur. The doctor can discuss anticipated treatment outcomes and the prognosis for long-term efficacy after performing a thorough medical history and examination.
Causes And Risk Factors
May-Thurner syndrome is random. It isnât something in your genes that you get from your parents.
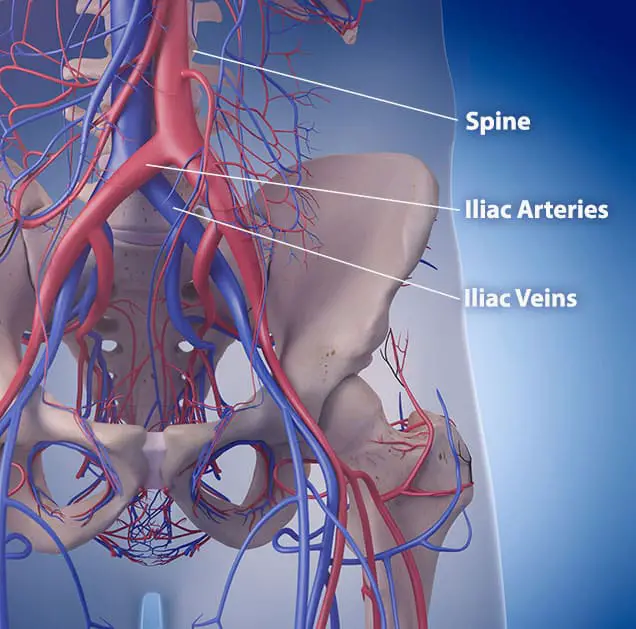
The crossover of those blood vessels is normal. But in some cases, they are positioned in a way that the right iliac artery presses the left iliac vein against the spine. That added pressure leaves a narrower opening. It can also lead to scars in the vein.
Youâre more likely to get May-Thurner syndrome if you:
- Venogram, a type of X-ray that uses a special dye to show the veins in your leg
Read Also: How To Heal Back Pain Quickly
Vein Specialists Of The Carolinas
All We Do Is Veins, All Day Every Day.
What Is May-Thurner Syndrome?
May-Thurner syndrome is basically vein symptoms from a blockage of the left leg vein as it goes through the pelvis. The LEFT leg VEIN gets squeezed between the RIGHT leg ARTERY and the spinal column. It can be very hard to tell what causes edema even with lots of medical testing.
Symptoms Include:
- Pain, heaviness, aching, restlessness, throbbing, varicose veins, leg swelling, leg discoloration or inflammation and leg ulcers.
- Pelvic, hip and back pain can be present
- Varicose veins in areas like the very upper inner thigh, on or underneath the buttock, in the groin area or lower body may be present
- Suspected when vein problems occur early in lifeteenage or early twenties. Classic example is tall thin teenage girl with swollen left leg
- It is one reason DVT is more common on the left
- Often found in those with lean body shape
The continued pulsation of the artery as it crosses over the vein and compresses it, cause inflammation and scarring in and around the vein. This narrows and blocks the outflow of the leg.
May-Thurner Was Thought To Be Rare
- Today, with better technology, we realize it was just rarely diagnosed
- We also have found it can occur on the right side
- There are 3 areas on each side that commonly get compressed
Since the veins from the pelvic organs, uterus, ovaries, bladder, rectum and gluteal muscles all drain into the leg veins, this blockage can affect them as well.
What Is Recovery From Surgery Like
Some of the surgeries associated with May-Thurner syndrome are done on an outpatient basis, meaning you can go home the same day after having them. You should be able to return to normal activities within a few days to a week.
For the more involved bypass surgery, youll have some soreness afterward. It may take several weeks to a couple of months to make a full recovery.
Your healthcare provider will instruct you on how often you need to follow up. If you have a stent, you may need an ultrasound check about a week after surgery, plus periodic monitoring after that.
Don’t Miss: Does Your Lower Back Hurt In Early Pregnancy
What Are Your Treatment Options
When an iliac vein narrowing is discovered, this can be treated with placement of a stent in the vein. The stent is inserted into the compressed iliac vein by a needle stick approach in the groin. The stent usually yields impressive improvements in the quality of life for those who have severe symptoms from iliac vein compression.
What Complications Are Associated With May

DVT is the main complication May-Thurner syndrome causes, but it can also have its own complications. When a blood clot in the leg breaks free, it can travel through the bloodstream. If it reaches your lungs, it can cause a blockage known as a pulmonary embolism.
This can be a life-threatening condition that requires emergency medical treatment.
Get immediate help if you experience:
Also Check: What Can Help Lower Back Pain
How Serious Is Iliac Vein Compression Syndrome
Iliac vein compression syndrome is a serious condition that affects two major blood vessels in the legs. Up to 25% of adults can be affected by IVCS, and it can be more with age. The condition is caused by a buildup of fluid in one or both of the veins that supply blood to the leg. This can lead to swelling, pain, numbness, tingling, or weakness.
It can also cause blood clots to form in these veins, which can block the flow of blood from one vein to another. In severe cases, the blood can become so diluted that it can no longer clot, leading to a life-threatening condition called a pulmonary embolism .
The most common symptoms are pain and tenderness in your legs and feet, as well as swelling and redness around the affected veins. These symptoms can last for a few days to several weeks. If you experience any of these symptoms, call your doctor right away.
What Are The Causes And Risk Factors Of May
May-Thurner syndrome is caused by the right iliac artery being on top of and putting pressure on the left iliac vein in your pelvis. Healthcare providers arent sure why this happens.
Its hard to know how many people have May-Thurner syndrome because it usually doesnt have any symptoms. However, according to a 2015 study, its estimated that of those who develop a DVT can attribute it to May-Thurner syndrome.
Per a 2018 study, May-Thurner syndrome occurs in women compared to men. Additionally, most cases of May-Thurner syndrome occur in individuals between ages 20 and 40, according to a 2013 case report and review.
Risk factors that can increase the risk for DVT in people with May-Thurner syndrome include:
- prolonged inactivity
Invasive tests:
- catheter-based venogram
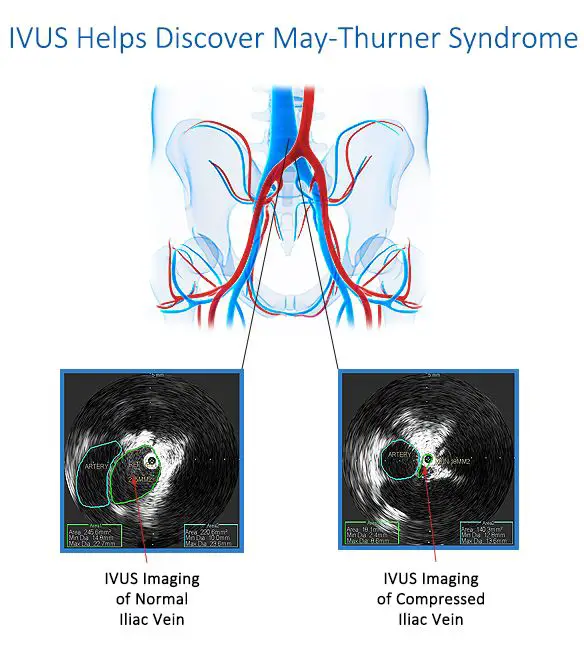
- intravascular ultrasound, which uses a catheter to perform an ultrasound from the inside of a blood vessel
Not everyone who has May-Thurner syndrome will know that they have it. However, the condition can require treatment if it starts to produce symptoms.
Its important to know that its possible to have May-Thurner syndrome without having DVT.
The reduction in blood flow associated with the narrowing of the left iliac vein can cause symptoms such as:
Recommended Reading: Why Is My Lower Back Pain Getting Worse
Chronic Pelvic Pain As An Unusual Presentation Of May
1Department of General Surgery, Sengkang General Hospital, Singapore 2Department of Vascular and Interventional Radiology, Singapore General Hospital, Singapore 3Department of Radiology, Sengkang General Hospital, Singapore 4Department of Vascular Surgery, Singapore General Hospital, Singapore. tang.tjun.yipsinghealth.com.sg
Dear Sir,
May-Thurner syndrome is described as venous outflow obstruction resulting from an anatomical variant in which the left common iliac vein is compressed by the right common iliac artery at the point of crossing over. Patients typically present with leg swelling and oedema or acute deep vein thrombosis at first presentation, with a smaller proportion presenting with pulmonary embolism. We herein report an unusual presentation of MTS in which the patient presented with chronic pelvic pain and bilateral intermittent lower limb swelling.
Understanding The Basics Of May
Do you have a history of deep vein thrombosis or persistent pain and swelling in your lower extremities? Have you or a loved one undergone hip or knee surgery but continue to experience leg swelling and difficulty walking. Have you had your veins treated without any resolution of your symptoms, or have the symptoms returned and are worse than ever? Do you have varicose veins in other places besides your lower extremities? Do you have pelvic pain or fullness and have been diagnosed with endometriosis, but the treatments that have been offered are not helping? If so, you may have May-Thurner syndrome. Also known as iliac vein compression, this condition can inhibit the flow of blood in your lower extremities.
Diego Hernandez, MD, of Bloomfield Vein & Vascular in Bloomfield Hills, Michigan, a Board Certified Vascular Surgeon, is an expert in vein conditions, and he can diagnose and treat not only deep vein thrombosis, but also the underlying causes, such as May-Thurner syndrome.
Read Also: Can Back Pain Be A Sign Of Breast Cancer
What Back Pain Treatment Options Are Available To Me May
There are many methods for treating back pain at home, but only a few of these have been proven to be effective. The most common treatment is rest and applying ice to the painful area. This treatment is very relaxing and should be used for only 10-20 minutes. It should never be applied while you sleep. Also, exercise and stretching exercises are essential for keeping muscles and supporting tissues flexible. While some of these methods may not seem like they are effective for you, they can help you overcome your back pain.
Physical therapy is a good option for treating back pain. It will help you improve your posture and strengthen your core muscles. Massage therapy and acupuncture are other options for relieving tension and reducing joint pain. Some people also find that water therapy improves flexibility and balance, while yoga helps them heal faster from injuries. Proper nutrition and lifestyle changes are also important for treating back pain. It is very important to consult a physician if you are experiencing back pain because it will help you avoid more serious conditions later on.
Outcome And Follow Up
The case was discussed at our Orthopaedic and Vascular multidisciplinary team meetings . The patient recovered well following a prolonged course of anticoagulation therapy with follow-up arranged to discuss with the patient the possibility of venoplasty and subsequent venous stenting. There has been no recurrence of DVT in the ensuing 6 months.
You May Like: Can A Chiropractor Help My Lower Back Pain
What Are The Symptoms Of May
Most people with May-Thurner syndrome dont experience any symptoms unless it causes deep vein thrombosis .
However, because May-Thurner syndrome can make it difficult for blood to circulate back to your heart, some people may experience symptoms without DVT.
These symptoms occur predominantly in the left leg and can include:
How Can I Prepare For Treatment
The doctor prescribes treatment based on the severity of the condition, the patient’s medical history, and other factors. Patients who are prescribed anticoagulant medication will have different pre-treatment recommendations that patients who undergo angioplasty and stenting. When treatment is discussed, the doctor will provide clear instructions regarding how to adequately prepare.
Don’t Miss: What Helps Arthritis In The Lower Back
What Is Venogram With Intervention
Veno means vein and Gram means picture. So, using ultrasound guidance our physicians inject dye into your veins and use X-ray technology to see the veins and assess their functionality to determine the correct treatment plan. Once the proper path is determined, a vein in either your arm, leg or neck is then perforated with a hallow needle, using ultrasound guidance. A wire is then advanced, under X-ray guidance, into the vein.
Next, depending on your need, possible interventions include:
In some cases, Intravascular ultrasound may also be used to evaluate the veins internally.