Stretch Crohns Lower Back Pain
Dont rest sagged in your workdesk chair all day. Stand up every 20 mins approximately as well as extend the other way. Due to the fact that the majority of us spend a lot of time flexing ahead in our tasks, its important to stand and also stretch backward throughout the day. Do not forget to likewise extend your legs. Some people find remedy for their back pain by doing a normal stretching regular, like yoga exercise. Crohns Lower Back Pain
Study Design And Data Collection
All IBD patients with and without self-reported joint/back pain, who signed informed consent, were seen at the JOINT outpatient clinic at study inclusion and at 1 year follow-up. During the 12-month study period, patients were asked to complete monthly questionnaires assessing IBD disease activity and spine and/or peripheral joint scores. When no response was received within 1 week, a reminder email or letter was sent out, followed by a telephone call.
Following the baseline assessment, patients were categorised into two study groups:
Patients with joint/back pain: CBP for 3 months and/or pJTC currently or during the previous year.
Patients without joint/back pain: no back pain or pJTC during the previous year.
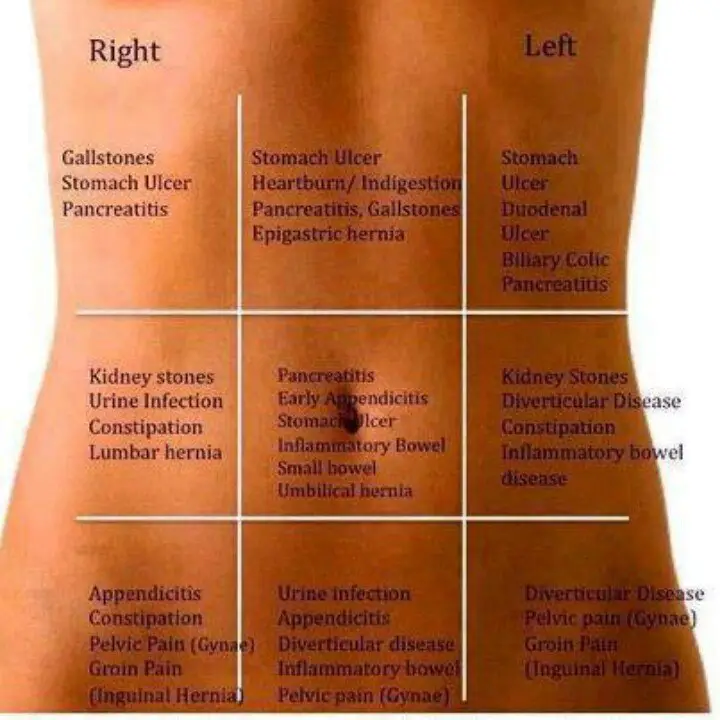
What Prevail Causes Of Lower Back Pain
Typical reasons for low back pain include lumbar stress, nerve inflammation, back radiculopathy, bony infringement, as well as conditions of the bone and joints. Each of these is evaluated below.
Back stress : A back pressure is a stretch injury to the ligaments, ligaments, and/or muscles of the lower back. The extending incident lead to tiny rips of varying levels in these cells. Back stress is thought about among the most usual sources of lower neck and back pain. Crohns Lower Back Pain
The injury can take place as a result of overuse, inappropriate usage, or injury. Soft-tissue injury is commonly classified as severe if it has actually existed for days to weeks. If the stress lasts longer than 3 months, it is referred to as chronic. Back stress usually occurs in individuals in their 40s, yet it can happen at any type of age. The condition is identified by localized pain in the lower back area with start after an occasion that mechanically emphasized the lumbar cells. The extent of the injury varies from light to serious, depending upon the degree of strain and also resulting spasm of the muscles of the lower back.
The medical diagnosis of back stress is based upon the history of injury, the place of the pain, as well as exemption of nerves injury. Usually, X-ray testing is just valuable to exclude bone irregularities.
Recommended Reading: Aleve Or Ibuprofen For Back Pain
Keep Your Bones Strong
Make sure you get enough calcium and vitamin D. Crohn’s disease makes bone loss and osteoporosis more likely. Steroids used to treat Crohn’s can also erode your bones. Most experts say you need between 1,000 and 1,300 milligrams of calcium and between 600 and 800 international units of vitamin D. Ask your doctor how much is right for you.
3
Diagnostic Tests/lab Tests/lab Values
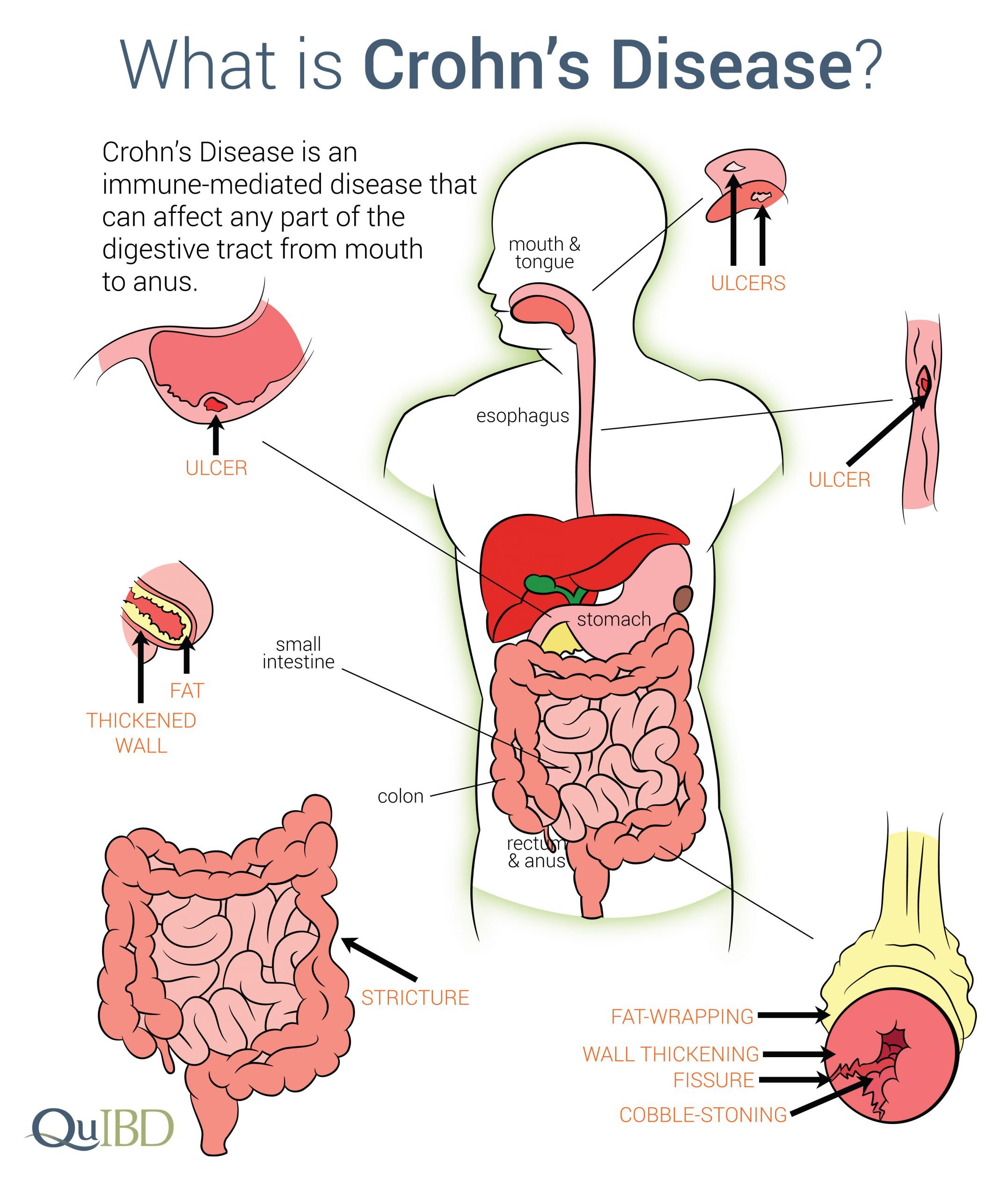
The diagnosis of Crohns disease is made by ruling out other potential causes to explain the patients signs and symptoms. Some of the tests include blood tests, fecal occult blood test , colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.
The blood tests are used to check for anemia which would indicate inflammation within the body, infection, and antibodies that might be present with individuals with inflammatory bowel disease.
The FOBT assesses an individuals stool sample for the presence of blood.
A colonoscopy allows the doctor to take a biopsy or tissue sample to determine if there is a presence of any granulomas which are common with Crohns disease and not ulcerative colitis.
The flexible sigmoidoscopy allows the doctor to assess the last portion of the colon for any biopsy samples. This allows the doctor to determine if there is any inflammation or bleeding amongst the intestines.
Barium enemas allow the doctors to assess the intestines via x-ray. The barium coats the inner lining of the GI tract to allow the lining to be visible on the x-ray.
A CT of the GI tract allows a quick look at the entire bowel in a way that cannot be seen in other diagnostic tests. This helps to assess for blockages, abscesses or fistulas.
You May Like: Does Aleve Work For Back Pain
What Is The Composition Of The Lower Back
To understand various root causes of lower back pain, it is necessary to value the normal style of the tissues of this location of the body. Crucial frameworks of the lower back that can be associated with signs and symptoms in this region include the bony lumbar spinal column , discs between the vertebrae, ligaments around the spine and also discs, spine as well as nerves, muscles of the lower back, interior body organs of the hips as well as abdominal area, and the skin covering the lumbar location. Crohns Lower Back Pain
The bony lumbar spine is designed to ensure that vertebrae stacked together can give a movable support framework while also protecting the spine from injury. The spinal cord is composed of worried tissue that prolongs down the spinal column from the brain.
Each vertebra has a spinous process, a bony importance behind the spine, which guards the cords anxious cells from impact injury. Spinal column additionally have a strong bony body in front of the spine to provide a system suitable for weight bearing of all tissues over the butts. The back vertebrae pile quickly atop the sacrum bone that is located in between the butts.On each side, the sacrum meets the iliac bone of the pelvis to form the sacroiliac joints of the butts.
What Are Nonsurgical Inflammatory Bowel Disease Treatments
IBD treatments vary depending on the particular type and symptoms. Medications can help control inflammation so you dont have symptoms . Medications to treat IBD include:
- Aminosalicylates minimize irritation to the intestines.
- Antibiotics treat infections and abscesses.
- Biologics interrupt signals from the immune system that cause inflammation.
- Corticosteroids, such as prednisone, keep the immune system in check and manage flares.
- Immunomodulators calm an overactive immune system.
You may also benefit from these over-the-counter IBD treatments:
- Antidiarrheal medication.
- Vitamins and supplements like probiotics.
You May Like: Is Aleve Or Ibuprofen Better For Back Pain
Trying Just About Anything
The acute pain went away after a few days, but the old pain, the usual pain, came and went with depressing regularity. Ibuprofen or naproxen helped but irritated his stomach. His primary-care doctor put him on Celebrex, which is easier on the gut. The medications, along with a cushion that he now had to carry with him everywhere, got him through the worst of the attacks. Every now and then, he would try a new specialist to see if anyone had anything new to offer. He saw a physical-medicine doctor, a neurologist, a pain specialist and finally an integrative-medicine doctor. They ordered imaging, physical therapy, massage therapy, injections, pills. He stopped his statin. He started yoga. Nothing really seemed to help much. So he stuck with his Celebrex and his cushion and his regular trips to the gym. He wasnt getting better, but he wasnt any worse either. The nighttime attacks of terrible pain were thankfully rare.
The doctor suffered for nearly a decade. Finally he found an answer and a treatment. But it didnt come through any of the experts he saw for his pain.
What Is Life Like With Ulcerative Colitis
The only cure for ulcerative colitis is complete surgical removal of the colon. However, most patients will not require surgery to have their symptoms under control, and some patients may have complications after the surgery such as pouchitis. Whether they require surgery or not, our goal is to allow our patients to live a full and productive life with ulcerative colitis. Most patients will require medications for an indefinite period of time. Research has shown that patients with ulcerative colitis who do not take their medication, even if they are feeling well, are more likely to have a return of their symptoms compared to patients who continue their medications. It is very important that patients discuss with their doctor if they are considering stopping their medications.
It is important for patients with ulcerative colitis, even if they are feeling well, maintain regular visits with their physician. For example:
- Patients on medications may need routine blood work to monitor for side effects.
- Patients with ulcerative colitis should keep up to date on immunizations including influenza , pneumococcal , human papilloma virus , and hepatitis A and B.
- Some patients with ulcerative colitis, particularly those who have had been exposed to steroids , may need to have bone mineral density tests to screen for early osteoporosis.
- Patients with ulcerative colitis will need to have colonoscopies to screen for colon cancer.
Also Check: Tylenol Or Aleve For Back Pain
Diagnosing Back Pain In Ulcerative Colitis
Diagnosing back pain as a symptom of ulcerative colitis can be tricky. Back pain can be attributed to a number of causes, including injury and strain. Because of the other potential causes, some people may not think to mention their backaches when seeking care for their UC. Whats more, back pain may develop years before UC does, making it more challenging to note the connection between the two.
If your doctor suspects that your UC has led to axial arthritis or ankylosing spondylitis, they will likely ask you to come in for a physical exam and tests. During this exam, they may test the range of motion in your spine and gauge your ability to take a deep breath. The doctor may also try to pinpoint the location of your pain by moving your legs or pressing on certain areas of your pelvis.
Radiographic tests are also commonly used to diagnose axial spondyloarthritis. Your doctor may use an X-ray to check for damage to your bones or joints. If no inflammatory damage is visible on the X-ray, your doctor may also order an MRI scan to get a more detailed view of your soft tissue and bones. An MRI scan can be particularly helpful, as it can allow doctors to catch and start treating your axial arthritis or AS before damage becomes extensive.
Lay Down Knees Bent Breathe
Lying on your back, knees bent, feet flat on the ground:
Put your hands on your ribs at the sides of your chest. Breathe in deeply through your nose and out through your mouth, pushing your ribs out against your hands as you breathe in. Repeat about 10 times. Remember, its as important to breathe out fully as it is to breathe in deeply.
Put your hands on the upper part of the front of your chest. Breathe in deeply through your nose and then breathe out as far as you can through your mouth. Push your ribs up against your hands as you breathe in again about 10 times. You can do this exercise at any time in a lying or sitting position.
Recommended Reading: Aleve Good For Back Pain
Other Ways To Treat Pain And Cramps
Sometimes, the pain is very difficult to control, even with medication. Your health care provider may suggest therapy or antidepressants in order to help you cope with the unrelenting pain.9
Antidepressants have not been well studied in people with inflammatory bowel disease. Therapy may improve anxiety, depression, and coping skills. However, it does not improve Crohn’s disease or ulcerative colitis.
What Are Surgical Treatments For Ulcerative Colitis
After 30+ years of living with ulcerative colitis, about 1 in 3 people need surgery.
A surgeon:
- Removes the colon or the colon and rectum .
- Connects the small intestine and anus.
- Creates an ileal pouch that collects stool, which then exits through the anus.
Rarely, you may need an ileostomy instead of an ileal pouch. An ileostomy bag attaches outside of the belly to collect stool.
A proctocolectomy is curative. Symptoms wont return after surgery to remove the colon and rectum. However, you may have problems with the ileostomy or ileal pouch, such as pouchitis .
Also Check: Advil Vs Ibuprofen For Back Pain
Ankylosing Spondylitis And Crohns Disease
When fusion occurs, axial spondyloarthritis progresses into ankylosing spondylitis . AS is a specific type of axial arthritis that causes inflammatory back pain and limits range of motion. If a persons AS causes significant fusing in the vertebral column and affects their rib movement, they may also struggle to take deep breaths.
Between 1 percent and 6 percent of people with Crohns disease also have ankylosing spondylitis. Although doctors arent entirely sure what causes AS, some research suggests a genetic component in the diseases development. Bowel or urinary tract infections are also believed to trigger the onset of AS in genetically susceptible people.
Inflammatory Spinal Disorders Common In Ibd Patients
NEW YORK Ankylosing spondylitis , axial spondyloarthritis and inflammatory back pain are common in inflammatory bowel disease patients two decades after IBD diagnosis, according to findings from the IBSEN study1.
You Might Also Like
Doctors should know IBD patients are at risk of inflammatory back problems, and refer them to a rheumatologist when appropriate, Dr. Alvilde Ossum of Oslo University Hospital in Norway, the studys first author, told Reuters Health in a telephone interview. It can actually damage the back more if you dont get help, she added.
While inflammatory back disorders are known to occur frequently in IBD patients, their prevalence is unclear, Dr. Ossum and her team note in the Journal of Crohns and Colitis, online September 13. To investigate, they looked at 470 patients participating in the Inflammatory Bowel South-Eastern Norway study, including 315 with ulcerative colitis and 156 with Crohns disease.
Twenty years after enrollment, 4.5% of study participants had AS, 7.7% had axial SpA, and 11.5% had inflammatory back pain, according to Assessment of Spondyloarthritis International Society criteria. AS prevalence in the general population is 0.26% in northern Norway and 0.25% in Europe, the researchers note, so the prevalence in IBD patients was 13 to 18 times higher.
Simple Tasks
ACR Convergence
Recommended Reading: How Much Advil Can I Take For Back Pain
Lower Back Pain With Ulcerative Colitis
Lower back pain and its relationship to inflammatory bowel disease has been talked about fairly often in our community. While there is no one reason for experiencing lower back pain , you are not alone if you experience this type of pain along with your Crohns disease or ulcerative colitis.
Before I continue, I want to reiterate that I am not a medical professional and if you are having this type of pain, I do highly suggest you bring it up to your doctor. There is often a reason for this pain that may require medical attention so I dont suggest waiting, if possible.
What Questions Should I Ask My Healthcare Provider
You may want to ask your healthcare provider:
- What type of IBD do I have?
- Whats the best treatment for me?
- What foods or drinks should I avoid?
- What lifestyle changes should I make?
- Am I at risk for other problems?
- Should I look out for signs of complications?
A note from Cleveland Clinic
Most people with inflammatory bowel disease enjoy active lives. Still, symptoms of Crohns disease and ulcerative colitis can be life-disrupting. Some people go into remission after taking medications. Some people need surgery to deal with severe symptom flare-ups. Your healthcare provider can suggest dietary and lifestyle changes to manage IBD.
Last reviewed by a Cleveland Clinic medical professional on 05/03/2021.
References
Don’t Miss: Does Motrin Help With Back Pain
Axial Spa According To Asas Criteria
Six patients had LBP and sacroiliitis on CT and/or MRE and responded to ASAS criteria for the diagnosis of axial SpA. Of these 6 patients, only one had inflammatory LBP. All these patients had CD. The 2 patients with negative HLA-B27 status did not meet the clinical criteria of axial SpA, while the HLA-B27-positive patient presented both inflammatory LBP and sacroiliitis on both digestive imaging methods.
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
Read Also: Advil Or Ibuprofen For Back Pain
Ankylosing Spondylitis And Ulcerative Colitis
When fusion occurs, axial spondyloarthritis progresses into ankylosing spondylitis. AS is a specific type of axial arthritis that causes inflammatory back pain and limits range of motion. If a person has AS that causes significant fusing in their vertebral column and affects their rib movement, they may also struggle to take deep breaths.
According to the University of Washington, ankylosing spondylitis symptoms generally dont present alongside gastrointestinal symptoms in people with UC. Although doctors arent entirely sure what causes AS, some research suggests a genetic component contributes to the diseases development. Bowel or urinary tract infections are also believed to trigger the onset of AS in genetically susceptible people.
Flares Obstructions Or Abscesses Impact Pain Levels
For many patients, abdominal pain gets worse when inflammatory bowel disease flares up.5 Active inflammation can cause pain.
Pain can also be a sign of an obstruction or abscess.3,5 However, people with IBD may have abdominal pain during remission, too. Inflammation can make the nerves more sensitive. It may cause lasting changes that contribute to pain during remission.5
Ongoing abdominal pain can impact your overall well-being.5 Fear of the pain can reduce your quality of life. Abdominal pain has been linked to depression in children and teenagers with IBD.6
Don’t Miss: Does Aleve Help With Back Pain