Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Functional Exercise For Chronic/persistent Pain
There are some simple exercises that you can try around the house to help:
- If you experience pain in your legs, keep them strong by practising standing up and sitting down in a chair.
- If your shoulders are aching, start by loosening them with some shoulder rolling actions, then by lifting an object that is slightly weighty from a shelf, and then replacing it. This increases the range of movement in your back, shoulders and arms, and then your strength.
Can The Sources Of Pain Be Pinpointed
Aware state surgical examination enables the patient to give the surgeon feedback, guiding him or her to the point that is responsible for the pain. This live approach allows the causal level in Parkinsons Syndrome Sufferers to be accurately defined and then viewed using endoscopic instruments through a tiny incision. In this way, neural anomalies and strange nerve combinations can be detected and diagnostic errors regarding the disc level responsible for the pain, avoided. Thus, the surgeon is guided to the precise source of pain at that specified inter-vertebral point and the understanding of the actual mechanisms underlying the causation of Parkinsons Syndrome Sufferers.
Don’t Miss: Does Aleve Work For Back Pain
Lower Back Pain And Parkinsons Disease
Lower back pain is an extremely common problem in the general population, as well as for people with Parkinsons disease . It tends to make moving more difficult, adding to the challenges of PD. Tim Nordahl, PT, DPT, a physical therapist at Boston University gave an excellent presentation as part of APDAs Lets Keep Moving Webinar Series. Because this is such a prevalent issue, and because there are things you can do to help alleviate your back pain, I wanted to summarize and highlight this important topic.
Revisiting Pain In Pdthe 50 Shades Of Pain Experienced By Parkinsons Patients
Pain is a quality of life issue for people with Parkinsons disease and can be under treated by doctors who may assume that is worsens as the disease progresses, although for some pain is an initial symptom of PD. This article helps focus your physicians attention in the right direction to accurately diagnose your pain.
Read Also: Advil Or Ibuprofen For Back Pain
James* Was Diagnosed With Parkinson’s In 2011 His Pain Has Worsened As His Condition Has Progressed
When I was diagnosed with Parkinson’s, I initially felt little to no pain. It’s only now, in the advanced stages of the condition, that I’ve started feeling pain, coupled with the normal ageing process.
One of the worst pains I experience is dystonia and dyskinesia of the upper body, especially in my neck and head. It usually starts with a pulsing headache, followed by jerking of the muscles in my face, neck, upper torso and hands. It’s particularly severe in my arthritic finger and my neck. It can be severe to mild, often very distressing, and can last up to 2 hours.
I also have mild to moderate, uncontrollable movements or swaying associated with dyskinesia. It’s more prominent when I’m sitting down at a table or working on my laptop. Strangely, I feel this pain at its worst when I’m on the phone, or trying to explain something, or if I’m feeling over-excited or anxious which is when I become severely dyskinetic. There’s now a dull, continuous pain in my neck, caused through the movement, which gets sharper during bouts of the symptom.
I also experience pain when standing, mostly during a ‘wearing off’ period. My knees pull towards each other and the pain is so severe that I can’t walk. Luckily it only lasts a minute or 2, but the pain can be distressing.
To ease the pain, I take paracetamol as and when, occasionally co-codamol, and very occasionally an anti-inflammatory, for the arthritis. I previously tried cannabis oil but it was of no benefit to me.
Negative Impact Of Severity Of Pain On Mood Social Life And General Activity In Parkinson’s Disease
This case control study designed for clinicians and rehabilitation specialists to effectively identify pain from the patient’s point of view determined that PD patients had significantly higher pain severity scores compared to controls. PD patients with depressive symptoms had significantly higher pain severity and pain interference scores than controls without depressive symptoms. PD patients reported greater scores on Global BPI pain interference and all components of the pain interference subscale. Therefore, PD and depression seem to be correlated with higher perceived pain, severity and interference. A report on this study, by Jose Marques Lopes, PhD., was published in Parkinson’s News Today, September 21, 2018.
You May Like: Ibuprofen For Back Pain Dosage
Pain Is A Common But Overlooked Problem In Parkinsons Disease
Pain is an often overlooked non-motor symptom of Parkinsons disease . Studies show that between 40-80% of people with PD report pain, which is likely why it is often suggested as a topic for this blog.
One of the reasons why the topic of pain and PD is difficult to address is that it is sometimes tough to discern whether a particular pain is due to PD or not. Chronic pain is such a common symptom among the general population, and people with PD are not immune to common problems as well. However, there are aspects of PD that may exacerbate the pain experienced from a common problem. In addition, there are particular types of pain that may be unique to people with PD.
Identify The Cause Of The Pain
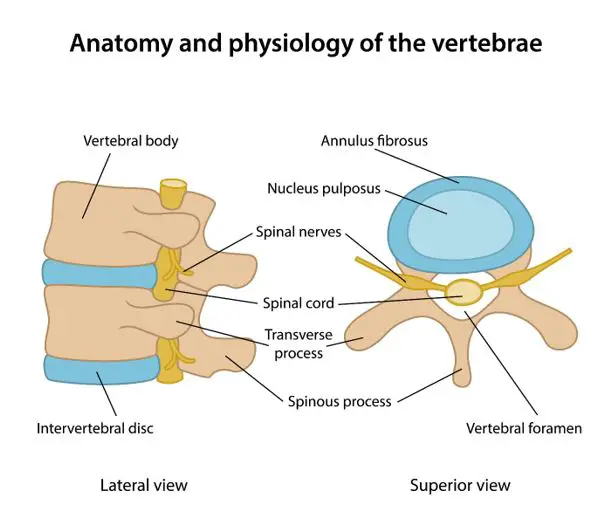
The first step in treating pain is to try to identify the cause. As I noted in the last essay, there are many different causes of pain for people with PD. If we look at the most common pain problems, low back and neck pain, we can see that there are many different causes for each. Many doctors order x-rays of the spine for these conditions, and they may be needed. The main problem with x-rays of the spine is that they always show arthritis, which is because virtually everyone over the age of 60 has arthritis in the spine. Whether thats the cause of the pain or not is usually not clear.
However, x-rays will show if theres a compression fracture , or a tumor. Since older women frequently develop compression fractures even without a fall, this can be important because we know then that the pain is likely severe, but time limited, and will resolve in a month or two. This makes it easier to treat with strong medication, like narcotics, because there is less concern for addiction. X-rays do not show discs, but disc herniation is much less common in older people so its of less concern.
Physical Therapy
Alternative treatments
Chiropractors focus entirely on spine pain and may be very helpful. Since many medical doctors are not very familiar with PD, I assume that many chiropractors probably arent either. Therefore it will be helpful to find one who is familiar with PD. Probably the best way to do this is through a Parkinsons Disease support group in your area.
Don’t Miss: How Much Advil For Back Pain
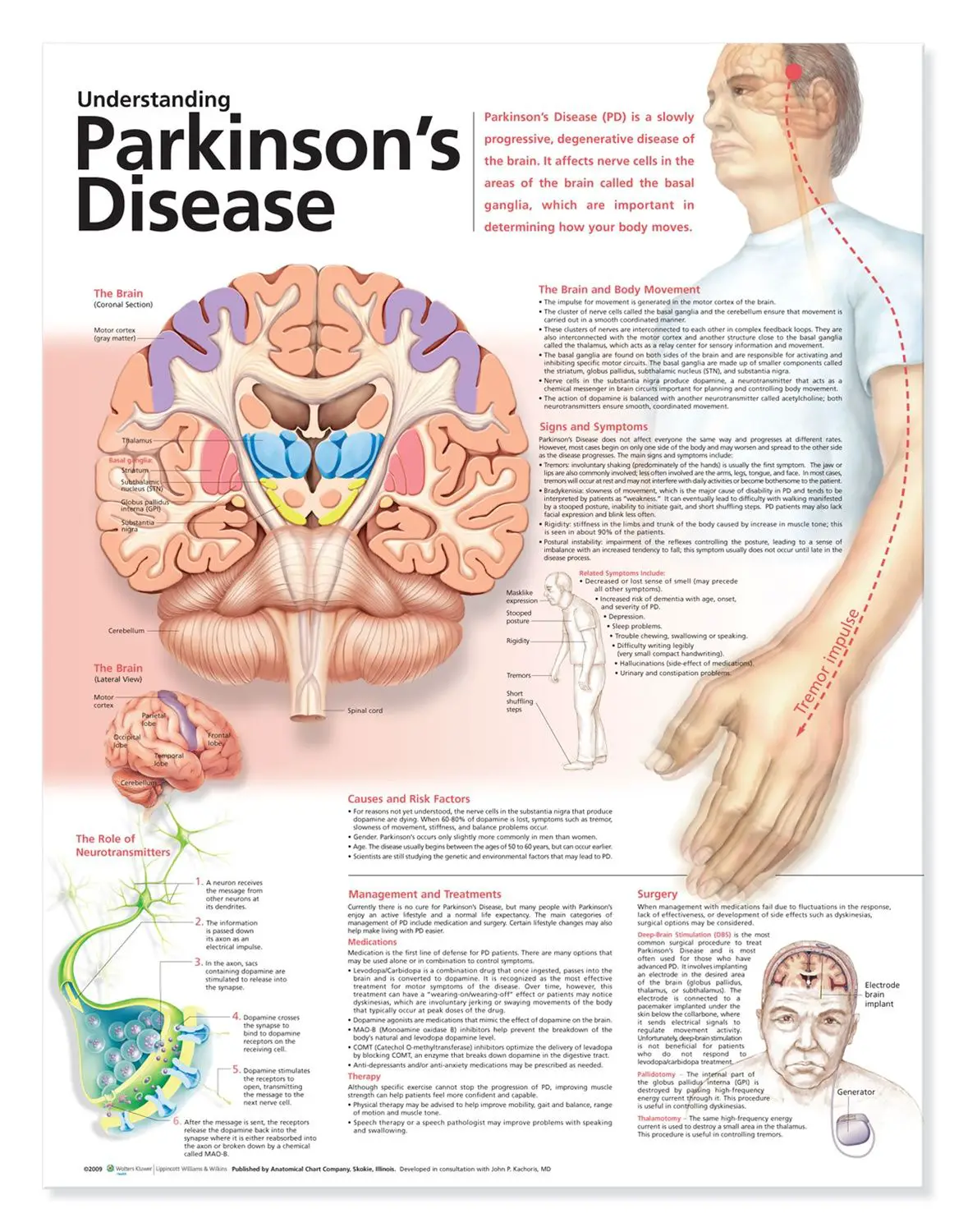
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Types Of Parkinson’s Pain
Most of the time, discomfort in muscles and joints is secondary to the motor features of Parkinsons lack of spontaneous movement, rigidity, and abnormalities of posture what is known as musculoskeletal pain. The most commonly painful sites are the back, legs, and shoulders and it is usually more predominant on the side more affected by parkinsonism.
But there are many other categories of pain associated with Parkinsons disease. Radicular or neuropathic pain is experienced as a sharp pain that can start in the neck or lower back with radiation to arm or leg respectively and is often associated with numbness or tingling, or a sensation of coolness in the affected limb. It is usually secondary to a pinched nerve due to something like a slipped disc.
Dystonia related pain occurs as its name suggests, at times of dystonia most often experienced in the foot, neck or face and arm at different points in the dosing schedule, particularly the off phase when there is not enough dopamine replacement but can uncommonly also occur at peak-dose times. It can be one of the most painful symptoms those with Parkinsons can face.
Akathisia pain is experienced as restlessness, a subjective inner urge to move, an inability to stay still and the inherent feelings of discomfort that it brings. It is primarily experienced in the lower limbs and can often be relieved by walking around.
Also Check: Will Aleve Help With Back Pain
Patient Disposition And Baseline Characteristics
Of 287 patients randomized , 246 completed the study 267 patients were included in the FAS, all of whom had baseline and follow-up Likert pain scale scores. At baseline, 187 patients with a Likert pain scale score 1 were considered to have any pain at baseline 100 patients with a Likert pain scale score 4 were considered to have moderate-to-severe pain . Of these patients, 21 reported severe pain this subgroup with severe pain was not investigated further due to the small sample size, but was included in the overall analyses. Patients with moderate-to-severe pain at baseline had higher baseline scores on UPDRS III and PDSS-2 than patients without pain .
Table 1 Demographic/baseline characteristics: by presence/absence of pain at baseline
Acpa And Stanford Resource Guide To Chronic Pain Management
This 213-page downloadable PDF is a comprehensive, integrated guide to medical, interventional, psychological/behavioral, pharmacologic, rehabilitative, complementary and integrative, and self-help strategies in the treatment of chronic pain. It covers general information compiled from multiple sources, is updated yearly and includes imbedded web links for certain medications and treatments and relevant internet sites of interest.
This questionnaire can help identify type of pain and determine whether someone should see a pain specialist.
Don’t Miss: Back Pain Cleveland Clinic
Gait & Balance Abnormalities
Parkinsons Disease Exam
Patients with Parkinsons disease can develop an alteration of the postural reflexes that causes instability in gait and balance control. Such alterations usually develop later in the course of the illness and are a major cause of disability, especially because of the high risk for falls that derives.
Using the exam to pick up postural instability is of the utmost importance for the management of patients with PD, since it will trigger either a medication adjustment or a physical therapy intervention both aimed at falls prevention.
We have three tests for this part of the PD exam:
1) Standing up from a chair
2) Free walking
3) Provoked pull test maneuver for balance
Mechanical Constraint Of Rigidity
Rigidity is one of the cardinal symptoms of PD and can be evident across axial, proximal, and distal body segments. Although largely neural rather than peripheral in its generation , the rigidity associated with PD elicits a significant mechanical constraint that associates with impaired gait quality , turning , standing postural sway , and diminished quality of life . Direct measurement of axial rigidity by slow, passive trunk or hip rotation in stance demonstrates an increased rigidity with PD that correlates with clinical symptom scores and with difficulty walking or rolling over . Thus, rigidity is a pervasive impairment in PD that influences mobility, balance, and daily life.
Recommended Reading: How Much Advil For Back Pain
Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
A total of 97 Parkinsons patients at a mean age of 67.7 years, including 60 men, and 97 individuals used as controls at a mean age of 67.5 years, including six men, without the disorder or other neuromuscular diseases, filled out a questionnaire on the intensity of local lumbar back pain. The intensity of leg radicular pain caused by inflammation and/or injury to a spinal nerve root was quantified by the visual analogue scale a continuous scale used to measure pain intensity.
In addition, the participants permanent functional disability was assessed via the Oswestry Low Back Pain Disability Questionnaire a self-completed questionnaire that includes 10 different topics: intensity of pain, lifting, ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality, and ability to travel.
Patients were further asked to describe the painful sensation they experience as pricking, tingling, burning, paresthesia often described as feelings of pins and needles, or numbness or other.
The team also assessed Parkinsons duration, medications being used, severity of motor symptoms as assessed by the Unified Parkinsons disease rating scale part III and the Hoehn and Yahr stage, which is a system used to assess symptom progression.
According to the ODI results, minimal disability was reported by 43.8% of Parkinsons patients, moderate disability by 27.5%, severe disability by 22.5%, and crippled by 6.3%.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Read Also: How Much Advil For Back Pain
Evaluating Lower Back Pain
When a person develops lower back pain, a neurological history and exam can help rule out serious medical conditions that may need further evaluation and intervention. The neurological history will collect information about other neurological symptoms such as numbness, tingling, weakness, new bowel or bladder symptoms, etc. The neurologic exam will assess strength, sensory changes and reflexes, among other things, which can shed light on spine function and help determine if a serious medical condition is present. Lower back pain caused by a serious medical condition is rare . Nevertheless, be sure to tell your neurologist about any new symptoms that you may have.
For most people, neurologic history and exam will confirm that lower back pain can be managed conservatively. When this is the case, treatment of the pain with exercise and physical therapy is the best course forward. Your neurologist may determine that imaging of the lower back will be helpful. If that is the case, he/she may order an MRI of the lower spine. An MRI will show structural changes to the lower spine but will not visualize PD-specific causes of lower back pain such as rigidity, dystonia, or central pain.
Studies have shown that MRIs can reveal structural changes that do not result in pain at all. So, it is important not to let imaging be the sole guidance of lower back pain management.
Sensory Acuity Kinesthesia And Dynamic Central Sensory Integration
Any type of physical activity optimally requires accurate sensation and perception of ones own position and movement , and both PD and LBP associate with impaired kinesthesia. People with PD exhibit impaired tactile sensation and impaired kinesthesia to detect limb position during active motion as well as to detect passive limb and trunk rotation . People with LBP exhibit impaired two-point discrimination and can be unable to kinesthetically perceive their lumbar trunk based on body image traces . In contrast to the global somatosensory impairment exhibited by people with PD, the impaired tactile discrimination of people with LBP appears to be isolated to the area of the LBP . Impaired lumbosacral repositioning accuracy has also been reported for people with LBP . Further, similar to the impaired detection of trunk motion exhibited by people with PD, people with LBP exhibit increased thresholds for detecting passive trunk flexion and lateral bending . Thus, although the extent of impairment may differ between people with PD versus LBP, both health conditions associate with impaired tactile acuity and kinesthesia.
Don’t Miss: How Much Advil For Back Pain
Lower Back Pain In People With Parkinsons
In a previous blog, we discussed pain and PD in general and highlighted different types of pain that a person with PD might experience.
PD contributes factors that can cause or worsen lower back pain, such as rigidity of the trunk muscles or dystonia of the trunk muscles. Both rigidity and dystonia can fluctuate with medication timing and correlate with ON and OFF time.
In addition, PD can be associated with central pain, which is poorly understood and thought to be due to abnormalities in the brain itself. Some new research suggests that PD can change how the brain feels pain that the loss of dopamine can make pain feel worse or make a person more likely to feel pain.
We know that:
- there is a higher prevalence of lower back pain in people with PD vs aged-matched controls
- certain features of PD such as increased age, depression, rigidity, and stooped posture are associated with lower back pain
- lower back pain can make it harder to deal with the challenges of PD because it is associated with lower activity levels. This can breed a vicious cycle in which lower back pain leads to decreased activity levels and then lower activity levels conspire to make the lower back pain worse