Can Constipation Cause Back Pain And Leg Pain At The Same Time
Leg pain on its own isnt usually caused by constipation. However, you may experience constipation with leg pain if your leg pain is also accompanied by back pain.
For example, you may have constipation if you have sciatica, which affects the sciatic nerves. The sciatic nerves run from your lower back through your hips and buttocks and down each leg. Sciatica occurs when pressure is being placed on one or both sciatic nerves and causes pain in the areas along the nerve, including the legs and back.
What Is The Best Food For Bowel Movements
What you consume either helps or hurts you unfortunately, there is not too much in-between. Eating the right types of food can improve your bowel movements.
For those with sciatica and other chronic pain and inflammation symptoms, making dietary changes can be crucial in reversing the severity of those symptoms.
Prunes are one of the most abundant sources of dietary fiber, which the human body requires.
As Lever, Cole, Scott, Emery, and Whelan found in their review of several studies, the consumption of prunes at a dosage level of 100 grams per day seems to be effective at improving the frequency and consistency of bowel movements. In fact, just one prune has an entire gram of fiber.
Another food to add to your diet to help improve bowel movements is a kiwi.
Kiwi is a fruit that lacks fructose, which is known to cause gas and bloating. A single cup of kiwi contains 5 grams of fiber, and kiwi is also loaded up with vitamin C.
Flaxseeds are tiny powerhouses when it comes to fiber. Just one tablespoon of flaxseeds contains 2 grams of fiber, and with how easily they can be mixed into meals, a little bit of flaxseed can go a long way in regulating bowel movements.
Just make sure that you dont eat flaxseeds whole since your body cannot properly digest them and garner enough of their nutrients that way.
One of the most important things that you can do to keep bowel movements regular is to drink enough water.
Why Do I Get A Sharp Pain In My Anus
Sharp pains in the anus are hard to identify in the absence of other symptoms. Pain while defecating can be caused by hemorrhoids or anal fissures. Pain following constipation can be due to rectal distension. To find the cause of sharp pains during defecation, it is necessary to examine associated symptoms individually. If you are experiencing sharp pains with no known cause, seek medical evaluation.
Read Also: Will Aleve Help Back Pain
I Get Terribly Embarrassed At Work Because I Cant Stop Burping And Farting How Can I Make It Stop
Excess belching can be the result of eating too quickly, drinking too quickly or drinking too many fizzy drinks. It can also be caused by nervousness, which makes people swallow a lot. The bicarbonate in saliva reacts with stomach acid to make CO2, which is then belched.
Excess farting may be due to eating too much fibre , or certain vegetables whose carbohydrate cant be digested by the human gut .
Extra-smelly farts are sometimes due to having too much fat in the diet. Fats may be broken down in the large bowel by bacteria, which produce volatile, unpleasant fatty acids.
Pain Or Discomfort In The Abdomen

What is it?
Abdominal pain or discomfort is one of the most common symptoms and one of the first symptoms to often present itself.
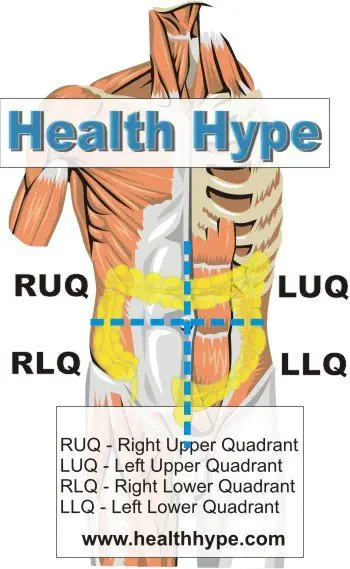
The pain or discomfort can be caused by the tumour invading nerves or organs that lie near the pancreas. The pain or discomfort is usually felt above the belly button and below the breast area , however, some patients report they have pain and discomfort without a specific location.
How do I know if I have this?
Having tummy pain or discomfort is a common symptom for many diseases and does not mean you have pancreatic cancer. However, if this is new and unusual for you or combined with other symptoms you should visit your GP to check.
Read Also: Ibuprofen For Back Pain Dosage
Chronic Or Recurrent Hemorrhoids
Chronic, or recurrent, hemorrhoids are swollen veins in the anus and rectum that never really resolve and may be symptomatic more or less constantly.
Hemorrhoids are caused by anything that puts pressure on the anus from the inside, such as straining during bowel movements constipation pregnancy or anal intercourse.
Most susceptible are pregnant women and older people, though anyone can be affected.
Symptoms include a small amount of bleeding during or after a bowel movement, as well as discomfort, itching, or swelling around the anus.
A medical provider can suggest treatment to ease the symptoms of chronic hemorrhoids, as well as make certain of the diagnosis since other, more serious conditions can have symptoms similar to hemorrhoids.
Diagnosis is made through patient history and physical examination.
Treatment most often involves simple lifestyle changes such as drinking more water adding fiber-rich foods to the diet using fiber supplements and stool softeners not delaying, or straining, to pass a bowel movement and using topical medications. Surgical procedures to remove the hemorrhoid can be used in some cases.
Rarity: Common
Top Symptoms: rectal bleeding, rectal pain, pain when passing stools, anal itching, painless rectal bleeding
Symptoms that never occur with chronic or recurrent hemorrhoids: unintentional weight loss
Urgency: Self-treatment
Common Accompanying Symptoms Of Rectal Pain
It is important to take note of the timing of the pain and any associated rectal pain symptoms, such as:
- Anal or rectal muscle spasms
- Incontinence
- Anal or rectal skin tags, bumps, or growths
- Open anal or rectal wounds
- Itchiness, burning, or sensitivity affected area
Rectal pain symptoms are often self-limited, meaning they go away on their own. However, if you frequently experience any of the above symptoms or they’re lasting, it is best to make an appointment with your doctor.
Don’t Miss: Is Advil Good For Back Pain
The Clinical Detective Game
There are a few ways to address this type of complex patient:
Profile the illness: This patient’s illness is manifested by a 6-month history of fatigue and weight loss, low back pain and morning stiffness for 4 years, decreased range of motion of the entire spine, probable left sacroiliitis, decreased chest expansion, abdominal pain and blood per rectum, anemia, thrombocytosis, and an elevated sedimentation rate and C-reactive protein.
Clinical designations: I would characterize this young man’s illness as chronic , systemic , inflammatory , progressive, and functionally limiting. Such labeling is of key importance because the timing, severity, ongoing, and expanding nature of the illness “educates” the differential diagnosis.
Develop a broad and well-thought-out differential diagnosis:The first is to think broadly about the illness. The differential diagnosis of a systemic inflammatory disorder must always initially include infection first because that needs to be addressed and treated immediately, cancer next for the same reason, and then a systemic inflammatory/autoimmune disorder.
Choose sentinel clinical manifestation: Sentinel, centrally important, clinical manifestations should jump out at you. These are defining manifestations around which the illness revolves or that are likely central to its pathology. In this patient they are low back pain and stiffness and persistent abdominal pain and blood in the stool.
Infection:
Inflammatory/autoimmune disorders:
Gas And Gastrointestinal Problems
Most of the time, gas is no more than a minor annoyance.
However, gas occasionally produces intense pain that makes the entire abdomen feel full and tender. This pain can radiate to the back, causing back pain and bloating. Minor gastrointestinal problems, such as stomach viruses, may also cause intense gas pain.
Sometimes, GI issues can cause muscle pain. This can happen after straining to have a bowel movement or repeatedly vomiting.
You May Like: Will Naproxen Help Back Pain
How Is Upper And Middle Back Pain Diagnosed
Your doctor will first ask you about your past health, your symptoms, and your work and physical activities. Then he or she will do a physical exam. Your doctor may also order an imaging test, such as an X-ray or an MRI, to find out if something such as a broken bone or a herniated disc is causing your pain.
You may need more tests to check for other possible causes for your pain.
Inflammatory Or Infectious Causes
Rectal pain may be the result of inflammation or infections, such as the following.
- Autoimmune disease: People with autoimmune diseases that affect the gastrointestinal tract, such as Crohn Disease or ulcerative colitis, can experience painful inflammatory episodes that cause rectal pain. Rectal ulcer syndrome is another cause of rectal inflammation that may be due to the immune system targeting the rectal tissue.
- Infection: A number of different viral, bacterial, and parasitic infections can lead to rectal pain. You are most susceptible if you engage in anal sex, travel to places where parasitic infections are endemic, or if you have any cuts in the anal or rectal area.
Don’t Miss: Mayo Clinic Lower Back Pain Exercises
Lower Back Pain And Digestive Health
Q1. Is almost constant lower back pain associated with ulcers or IBS? Pain often keeps me awake at night then at times I can go for days with none. But I have back pain 80 percent of the time. I also have a lot of indigestion, belching, and gas.
Donis, Virginia
Persistent back pain, as you describe, is rare with common gastrointestinal disorders like peptic ulcer disease or irritable bowel syndrome . Ulcers can cause pain, but usually in the front region of the abdomen, known as the epigastrium. When an ulcer is very severe, it can perforate the wall of the duodenum and stomach and cause referred pain to many regions, including the back. However, perforation is a serious complication and would not continue for days or weeks without leading to more severe illness. If perforation is suspected, early imaging and treatment are performed surgical drainage or resection is often required.
IBS leads to bloating and changes in bowel habits , but back pain, while occasionally present in IBS, would not be a characteristic feature.
Other gastrointestinal disorders that can cause back pain along with indigestion include pancreatitis and diverticulitis, and I would recommend that you return to your gastroenterologist to get blood tests and imaging tests to test for these relatively common conditions.
Margaret, Texas
In summary, you don’t need to worry about eating foods to try to change the pH of your digestive system your body will do it for you!
When To See Your Doctor
If you notice any colorectal cancer symptoms persistent, quickly make an appointment with an oncologist. Talk to your doctor about the symptoms, and the doctor will recommend you image tests and begin screening for colon cancer. If you have a family history of cancer, then get yourself diagnosed and screened for colon cancer.
Read Also: Aleve Lower Back Pain
Go Deepertheres A Lot More To Discover About Ibs
IFFGDs publications are written by noted doctors and therapists from around the world. Here are some suggestions: Gynecological Aspects of IBS looks at IBS features in women. IBS in Men: A Different Disease? looks at IBS features in men. We have many publications about IBS available as PDFs in our library.
The Rome IV Diagnostic Criteria*
for IBS is as follows:
Recurrent abdominal pain, on average, at least 1 day per week in the last 3 months, associated with 2 or more of the following criteria:
What It All Means
The pain and symptoms of colon cancer arent always obvious. A dull bellyache that persists may be a warning sign. Consistent cramps may be a reason to visit a doctor. Early prevention is the most important factor when it comes to surviving colon cancer. Your best defense is regular screenings, even if you are under 55. Diet and lifestyle matter. A typical western diet, sedentary lifestyle and imbalanced gut all increase the risk of developing colon cancer. Staying active, eating a healthful and balanced diet, and increasing your vegetable intake are all protective measures.
Colon cancer is not a death sentence. Researchers are constantly improving treatment options, and complimentary therapies to improve both survival rates and quality of life.
Also Check: Is Aleve Good For Back Pain
Ibs Jaw And Face Pain
IBS can be such a pain in the…face? The research suggests that people with IBS are at a greater risk of experiencing joint and face pain due to a higher likelihood of experiencing other centralized chronic pain conditions.
One recent study showed that people with any subtype of IBS were three times more likely to experience pain and compromised movement of the jaw joint and the surrounding muscles due to Temporomandibular disorders .
According to John Hopkins Medicine, TMDs are disorders of the jaw muscles, temporomandibular joints , and the nerves associated with chronic facial pain.
Similar to IBS, current research suggests that hypnosis may also be an effective tool for treating TMD pain. â
Pain That Doesnt Disappear After Bowel Movement
Your lower back pain should disappear after a bowel movement, since that alleviates any pressure you may be experiencing in your pelvic area. However, if the pain persists or intensifies after your bowel movement, it could be a sign that a nerve was pinched or something was dislodged when your colon loosened up.
You May Like: Back Pain Cleveland Clinic
What Causes Upper And Middle Back Pain
Upper and middle back pain may be caused by:
- Overuse, muscle strain, or injury to the muscles, ligaments, and discs that support your spine.
- Poor posture.
- Pressure on thespinal nerves from certain problems, such as a herniated disc.
- A fracture of one of the vertebrae.
- Osteoarthritis caused by the breakdown of cartilage that cushions the small facet joints in the spine.
- Myofascial pain that affects the connective tissue of a muscle or group of muscles.
In rare cases, pain may be caused by other problems, such as gallbladder disease, cancer, or an infection.
Treatment If Back Pain Gets Worse
If your back pain doesn’t get better or it gets worse, your doctor may recommend:
- Prescription medicines, such as opioids, to help reduce pain.
- Muscle relaxants to help reduce pain and muscle tension and improve mobility. These can help with severe muscle spasms that happen when the back pain starts .
- Antidepressants, such duloxetine, to help treat long-lasting back pain.
- Steroid shots to help reduce swelling and relieve pressure on nerves and nerve roots. But there is little evidence showing that these shots can help control back pain.
In some cases, a back brace may be used to support the bones in the spine after a fracture.
Surgery is seldom used to treat upper and middle back pain. If your doctor recommends surgery, the type will depend on the problem you have. Surgery choices may include:
Read Also: Does Aleve Help Back Pain
Can Sciatica Affect Your Bowels
One of the most common symptoms of sciatica is a change in bowel movements.
Many who experience the searing pain of sciatica also deal with severe constipation.
Dr. Shannon Thieroff writes that not only does sciatica cause constipation, but it can lead to a loss of bowel control when the condition develops into cauda equina syndrome, which is the result of damage done to the nerve bundles located at the bottom of your spinal cord.
Oftentimes, constipation pre-dates sciatic nerve pain and is something that many patients do not seek treatment for early on. Stress and eating habits tend to play a role in the development of constipation as your gut flora becomes increasingly unhealthy.
What Causes Back Pain In Ulcerative Colitis

- Fatigue
- Weight loss
A person having backaches may not realize its related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
Don’t Miss: Mayo Clinic Low Back Pain Exercises
Ibs Headache And Migraine Pain
How can an irritable gut make your head irritable too? Head pain and gut pain may seem like an unlikely pair, but science shows that people with IBS also commonly experience migraines and headaches.
A study published in the Polish Journal of Neurology and Neurosurgery showed that between 23 to 53 percent of people with IBS experienced frequent headaches. Additional research, published in the Journal of BMC Gastroenterology, reported that people with IBS were around 60% percent more likely to experience migraines than people without IBS.
The connection between the gut and the head works both ways. Just as people with IBS often have headaches, people with migraines often experience gastrointestinal symptoms associated with IBS during a migraine attack.
Why Do I Have Rectal Pain When I Poop
Rectal pain may be caused by many things. You should consider what kind of stool you are having as well as if there is blood present. The presence of blood is often a sign of a small tear, called an anal fissure, which can be painful or burning. Proctalgia fugax is a rarer cause in which the muscles of the anus and rectum spasm in association with pain.
You May Like: How Much Advil Can I Take For Back Pain